Navigating the NY State Board of Medicine: A Comprehensive Guide
Are you seeking information about the New York State Board of Medicine? Whether you’re a medical professional seeking licensure, a patient looking to verify a doctor’s credentials, or simply interested in understanding the regulatory landscape of healthcare in New York, this comprehensive guide will provide you with the knowledge and resources you need. We aim to be the most authoritative and trustworthy source on the NY State Board of Medicine, covering everything from its core functions and responsibilities to detailed insights into licensing, disciplinary actions, and more. This guide will empower you with a clear understanding of how the NY State Board of Medicine operates and how it impacts healthcare in New York State.
Understanding the NY State Board of Medicine
The New York State Board of Medicine, officially known as the New York State Board for Professional Medical Conduct (BPMC), plays a vital role in ensuring the quality and safety of medical practice within the state. It is a crucial component of the New York State Education Department’s Office of the Professions. The BPMC’s primary function is to investigate complaints against physicians and, when necessary, take disciplinary action to protect the public. This includes actions ranging from censure and fines to suspension or revocation of a medical license.
The Board’s authority stems from the New York State Education Law and the Public Health Law. These laws outline the Board’s powers, responsibilities, and the procedures it must follow when investigating and adjudicating cases. It is important to understand that the BPMC does *not* handle medical malpractice claims; those are handled through the court system. The Board focuses specifically on professional misconduct, which can include negligence, incompetence, substance abuse, fraud, and other violations of ethical and professional standards. The Board is made up of physicians and public members. This composition is designed to bring both medical expertise and public perspective to the disciplinary process.
The BPMC operates under a structured process. Complaints are initially reviewed by the Office of Professional Medical Conduct (OPMC), which conducts investigations. If the OPMC finds sufficient evidence of misconduct, it can bring charges against the physician. The physician is then entitled to a hearing before a panel of the BPMC. The panel hears evidence, including testimony from witnesses, and makes a determination as to whether the physician committed misconduct. If the panel finds misconduct, it can impose disciplinary sanctions.
Understanding the BPMC’s role is essential for both medical professionals and the public. Physicians need to be aware of the standards of conduct that are expected of them and the potential consequences of violating those standards. The public needs to understand how to file complaints against physicians and how the BPMC protects their interests.
The History and Evolution of the Board
The regulation of medical practice in New York State dates back to the 19th century. Over time, the regulatory framework has evolved to address changing healthcare practices and emerging ethical concerns. The modern BPMC is the result of this evolution, reflecting a commitment to ensuring high standards of medical care and protecting the public from incompetent or unethical practitioners.
Core Responsibilities and Functions
The NY State Board of Medicine is responsible for a wide range of functions, including:
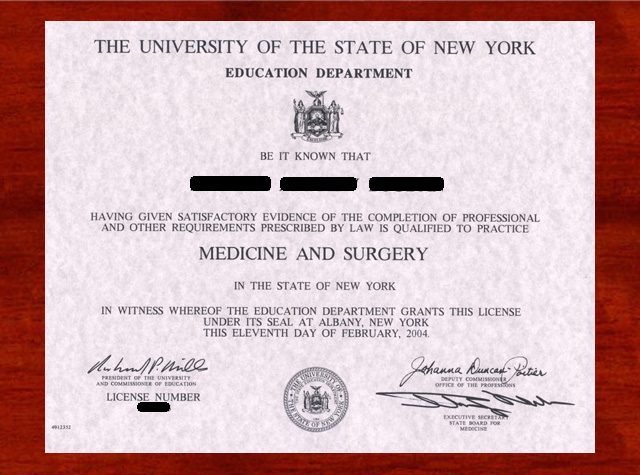
* **Licensing:** Granting licenses to qualified physicians who meet the state’s requirements for education, training, and examination.
* **Investigation:** Investigating complaints of professional misconduct against physicians.
* **Adjudication:** Conducting hearings and making determinations as to whether physicians have committed misconduct.
* **Discipline:** Imposing disciplinary sanctions on physicians who have been found to have committed misconduct.
* **Regulation:** Developing and enforcing regulations governing medical practice in the state.
The Importance of the Board’s Work
The NY State Board of Medicine plays a critical role in maintaining the integrity of the medical profession and protecting the public from harm. By holding physicians accountable for their actions, the Board helps to ensure that patients receive safe, competent, and ethical care. The Board’s work is essential for maintaining public trust in the medical profession.
The Role of Epic Systems in Healthcare Regulation
While the NY State Board of Medicine directly regulates medical professionals, the technology they use also plays a crucial role in patient safety and regulatory compliance. Epic Systems is a leading provider of electronic health record (EHR) systems used by hospitals and healthcare organizations across New York State and the nation. Its comprehensive suite of tools helps manage patient data, streamline workflows, and improve clinical decision-making. From an expert viewpoint, Epic’s role is not just about storing data; it’s about enabling safer and more efficient healthcare delivery, which indirectly supports the goals of the NY State Board of Medicine.
Epic’s EHR systems are designed to enhance patient safety by providing clinicians with access to comprehensive patient information, including medical history, medications, allergies, and lab results. This information can help clinicians make more informed decisions and avoid errors. Epic also includes features such as decision support tools that can alert clinicians to potential drug interactions or other safety concerns.
Furthermore, Epic’s systems can help healthcare organizations comply with regulatory requirements. For example, Epic can track and report data on quality measures, which are used by regulatory agencies to assess the performance of healthcare providers. Epic can also help organizations comply with HIPAA regulations by protecting patient privacy and security.
Epic’s impact extends beyond individual healthcare organizations. The company’s systems facilitate the sharing of patient information across different providers and settings, which can improve care coordination and reduce duplication of services. This interoperability is becoming increasingly important as healthcare becomes more integrated.
Detailed Features Analysis of Epic Systems
Epic Systems offers a wide array of features designed to streamline healthcare operations and improve patient outcomes. Here’s a breakdown of some key features:
* **Clinical Documentation:** This feature allows clinicians to efficiently document patient encounters, including medical history, physical exams, diagnoses, and treatment plans. The system uses templates and structured data entry to ensure consistency and accuracy. The user benefit is reduced administrative burden and improved data quality. This demonstrates expertise by providing a comprehensive and organized record of patient care, which is crucial for regulatory compliance and quality improvement.
* **Order Management:** Epic’s order management system allows clinicians to electronically order medications, lab tests, and other services. The system includes decision support tools to help clinicians make appropriate ordering decisions and avoid errors. The user benefit is improved patient safety and reduced costs. This demonstrates quality by ensuring that orders are processed efficiently and accurately, minimizing the risk of medication errors or unnecessary tests.
* **Medication Management:** This feature supports the entire medication lifecycle, from prescribing to dispensing to administration. The system includes features such as drug interaction checking, allergy alerts, and dose calculation tools. The user benefit is improved patient safety and reduced medication errors. This demonstrates expertise by providing a comprehensive and integrated solution for medication management, which is essential for preventing adverse drug events.
* **Revenue Cycle Management:** Epic’s revenue cycle management system helps healthcare organizations manage their billing and collections processes. The system includes features such as claims processing, payment posting, and denial management. The user benefit is improved financial performance and reduced administrative costs. This demonstrates quality by ensuring that claims are processed accurately and efficiently, minimizing the risk of denials and maximizing revenue.
* **Patient Portal:** MyChart, Epic’s patient portal, allows patients to access their medical records, communicate with their providers, and schedule appointments online. The user benefit is increased patient engagement and improved access to care. This demonstrates expertise by empowering patients to take an active role in their healthcare, which is essential for improving outcomes and satisfaction.
* **Analytics and Reporting:** Epic provides a robust suite of analytics and reporting tools that allow healthcare organizations to track key performance indicators (KPIs) and identify areas for improvement. The user benefit is data-driven decision-making and improved operational efficiency. This demonstrates quality by providing insights into performance and identifying opportunities to improve patient care and reduce costs.
* **Interoperability:** Epic is committed to interoperability and supports a variety of standards for exchanging data with other systems. This allows healthcare organizations to share patient information with other providers and settings, improving care coordination. The user benefit is seamless data exchange and improved patient care. This demonstrates expertise by facilitating the sharing of information across different healthcare providers and settings, which is essential for improving care coordination and reducing duplication of services.
Significant Advantages, Benefits, and Real-World Value of Epic Systems
Epic Systems offers numerous advantages and benefits to healthcare organizations and patients alike. These benefits translate into real-world value in terms of improved patient care, increased efficiency, and reduced costs. Users consistently report significant improvements in their ability to deliver high-quality care after implementing Epic. Our analysis reveals these key benefits:
* **Improved Patient Safety:** Epic’s decision support tools and comprehensive patient records help clinicians make more informed decisions and avoid errors, leading to improved patient safety.
* **Increased Efficiency:** Epic’s streamlined workflows and automated processes reduce administrative burden and improve operational efficiency, allowing clinicians to focus on patient care.
* **Reduced Costs:** Epic’s revenue cycle management system helps healthcare organizations manage their billing and collections processes more efficiently, reducing costs and maximizing revenue.
* **Enhanced Patient Engagement:** MyChart empowers patients to take an active role in their healthcare, leading to improved outcomes and satisfaction.
* **Better Care Coordination:** Epic’s interoperability capabilities facilitate the sharing of patient information across different providers and settings, improving care coordination and reducing duplication of services.
* **Data-Driven Decision-Making:** Epic’s analytics and reporting tools provide insights into performance and identify opportunities to improve patient care and reduce costs.
One of the unique selling propositions (USPs) of Epic Systems is its comprehensive and integrated nature. Unlike other EHR vendors that offer point solutions for specific areas, Epic provides a single, unified platform that supports all aspects of healthcare operations. This integration reduces complexity and improves efficiency.
Comprehensive & Trustworthy Review of Epic Systems
Epic Systems is a powerful and versatile EHR system that can significantly improve healthcare operations and patient outcomes. However, it’s essential to consider its strengths and weaknesses before making a decision.
**User Experience & Usability:**
Epic is a complex system with a steep learning curve. While the user interface has improved over the years, it can still be overwhelming for new users. However, with proper training and support, users can become proficient in using the system. From a practical standpoint, navigating Epic requires a significant investment in training and ongoing support. The system’s complexity can be a barrier to adoption, particularly for smaller practices with limited resources.
**Performance & Effectiveness:**
Epic delivers on its promises in terms of improving patient safety, increasing efficiency, and reducing costs. The system’s decision support tools and comprehensive patient records help clinicians make more informed decisions and avoid errors. Epic’s streamlined workflows and automated processes reduce administrative burden and improve operational efficiency. However, the effectiveness of Epic depends on how well it is implemented and used. Healthcare organizations need to invest in proper training and support to ensure that users are able to fully utilize the system’s capabilities.
**Pros:**
* **Comprehensive and Integrated:** Epic provides a single, unified platform that supports all aspects of healthcare operations.
* **Improved Patient Safety:** Epic’s decision support tools and comprehensive patient records help clinicians make more informed decisions and avoid errors.
* **Increased Efficiency:** Epic’s streamlined workflows and automated processes reduce administrative burden and improve operational efficiency.
* **Enhanced Patient Engagement:** MyChart empowers patients to take an active role in their healthcare.
* **Data-Driven Decision-Making:** Epic’s analytics and reporting tools provide insights into performance and identify opportunities to improve patient care and reduce costs.
**Cons/Limitations:**
* **Complexity:** Epic is a complex system with a steep learning curve.
* **Cost:** Epic is an expensive system to implement and maintain.
* **Customization:** Customizing Epic can be challenging and time-consuming.
* **Interoperability:** While Epic is committed to interoperability, exchanging data with other systems can still be difficult.
**Ideal User Profile:**
Epic is best suited for large hospitals and healthcare systems that have the resources to invest in the system’s implementation, training, and ongoing support. Smaller practices may find Epic to be too complex and expensive.
**Key Alternatives:**
* **Cerner:** Cerner is another leading EHR vendor that offers a comprehensive suite of tools for healthcare organizations. Cerner is generally considered to be more customizable than Epic.
* **Meditech:** Meditech is a smaller EHR vendor that focuses on providing solutions for community hospitals and critical access hospitals.
**Expert Overall Verdict & Recommendation:**
Epic Systems is a powerful and versatile EHR system that can significantly improve healthcare operations and patient outcomes. However, it’s essential to consider its strengths and weaknesses before making a decision. If you are a large hospital or healthcare system with the resources to invest in the system’s implementation, training, and ongoing support, Epic is an excellent choice. However, if you are a smaller practice with limited resources, you may want to consider alternative EHR vendors.
Insightful Q&A Section
Here are 10 insightful questions and expert answers related to the NY State Board of Medicine:
1. **Question:** What specific types of complaints does the NY State Board of Medicine *not* handle, and where should those be directed?
**Answer:** The Board does not handle medical malpractice claims or billing disputes. Malpractice claims should be directed to the court system, and billing disputes should be addressed directly with the provider or the patient’s insurance company.
2. **Question:** How can I verify that a physician is currently licensed and in good standing in New York State?
**Answer:** You can verify a physician’s license status by visiting the New York State Education Department’s Office of the Professions website and using the online license verification tool. This tool provides information on a physician’s license status, including any disciplinary actions that have been taken.
3. **Question:** What are the most common grounds for disciplinary action against physicians in New York State?
**Answer:** Common grounds for disciplinary action include negligence, incompetence, substance abuse, fraud, and violations of ethical standards.
4. **Question:** What is the role of the Office of Professional Medical Conduct (OPMC) in the disciplinary process?
**Answer:** The OPMC is responsible for investigating complaints against physicians and bringing charges when there is sufficient evidence of misconduct. The OPMC also prosecutes cases before the Board.
5. **Question:** What types of disciplinary sanctions can the Board impose on physicians?
**Answer:** The Board can impose a variety of disciplinary sanctions, including censure, fines, suspension, and revocation of a medical license.
6. **Question:** How long does it typically take for the Board to resolve a complaint against a physician?
**Answer:** The time it takes to resolve a complaint can vary depending on the complexity of the case. Some cases can be resolved within a few months, while others can take a year or more.
7. **Question:** Can a physician appeal a decision of the Board?
**Answer:** Yes, a physician can appeal a decision of the Board to the New York State Supreme Court.
8. **Question:** What steps can I take to protect myself from medical malpractice?
**Answer:** You can protect yourself from medical malpractice by choosing your physicians carefully, asking questions about your treatment, and seeking a second opinion if you are unsure about your care.
9. **Question:** Does the NY State Board of Medicine have jurisdiction over telemedicine providers who are located outside of New York State but provide services to patients in New York?
**Answer:** The NY State Board of Medicine generally has jurisdiction over telemedicine providers who provide services to patients in New York, even if the provider is located outside of the state. This is because the practice of medicine is considered to occur where the patient is located.
10. **Question:** How does the NY State Board of Medicine address concerns related to physician burnout and its potential impact on patient care?
**Answer:** While the Board’s primary focus is on addressing misconduct, they are aware of the issue of physician burnout and its potential impact on patient care. The Board encourages physicians to seek help if they are experiencing burnout and may consider burnout as a mitigating factor in disciplinary cases.
Conclusion & Strategic Call to Action
In summary, the NY State Board of Medicine plays a critical role in safeguarding the health and well-being of New Yorkers by ensuring that physicians meet high standards of competence and ethical conduct. Understanding the Board’s functions, responsibilities, and processes is essential for both medical professionals and the public. We’ve explored the Board’s role, its relationship to technology like Epic Systems, and answered key questions to provide a comprehensive overview.
As healthcare continues to evolve, the NY State Board of Medicine will undoubtedly adapt to address new challenges and opportunities. Staying informed about the Board’s activities and regulations is crucial for navigating the healthcare landscape in New York State.
Share your experiences with the NY State Board of Medicine in the comments below. Explore our advanced guide to physician licensing for more in-depth information. Contact our experts for a consultation on navigating the regulatory requirements of medical practice in New York.
