Understanding the NYS Medicaid Formulary: A Comprehensive Guide
Navigating the healthcare system can be complex, especially when it comes to understanding which medications are covered by your insurance. For New York residents relying on Medicaid, the NYS Medicaid Formulary is a crucial resource. This comprehensive list dictates which prescription and over-the-counter drugs are covered under the NYS Medicaid program. This guide aims to provide an in-depth understanding of the NYS Medicaid Formulary, making it easier for you to access the medications you need. We’ll explore its core components, how it works, and how to navigate it effectively, ensuring you can make informed decisions about your healthcare. This is your one-stop resource for understanding the NYS Medicaid formulary.
We’ll delve into the specifics of the formulary, including its different tiers, coverage rules, and exceptions. We’ll also explore how the formulary impacts your access to medications and what options are available if a medication you need isn’t covered. Our goal is to empower you with the knowledge and tools to navigate the NYS Medicaid Formulary with confidence.
With years of experience assisting patients with navigating the complexities of healthcare coverage, we’ve seen firsthand the challenges individuals face when trying to understand their medication benefits. This guide is designed to cut through the jargon and provide clear, actionable information, ensuring you can access the medications you need without unnecessary stress or confusion.
What is the NYS Medicaid Formulary? A Deep Dive
The NYS Medicaid Formulary, often referred to simply as the “formulary,” is a list of prescription and over-the-counter medications covered by New York State’s Medicaid program. It’s essentially a blueprint for medication coverage, guiding both patients and healthcare providers in making cost-effective and clinically appropriate treatment decisions. Understanding its nuances is key to maximizing your healthcare benefits.
The formulary isn’t a static document; it’s regularly updated to reflect new medications, changing medical guidelines, and cost considerations. The New York State Department of Health, in conjunction with a Pharmacy and Therapeutics (P&T) Committee comprised of physicians, pharmacists, and other healthcare professionals, reviews and revises the formulary. This ensures that the formulary remains current and aligned with the latest evidence-based practices.
The formulary typically includes multiple tiers, each representing a different cost level for the patient. Lower tiers generally consist of generic medications, while higher tiers may include brand-name drugs or specialty medications. The tier a medication falls into directly impacts the copay or cost-sharing amount the patient is responsible for.
Core Concepts and Advanced Principles
Understanding the core concepts of the NYS Medicaid Formulary is essential for effective navigation. Here are some key principles:
- Tiered System: Medications are categorized into different tiers, each with a different cost-sharing amount. Generic drugs are usually in lower tiers with lower copays, while brand-name and specialty drugs are in higher tiers with higher copays.
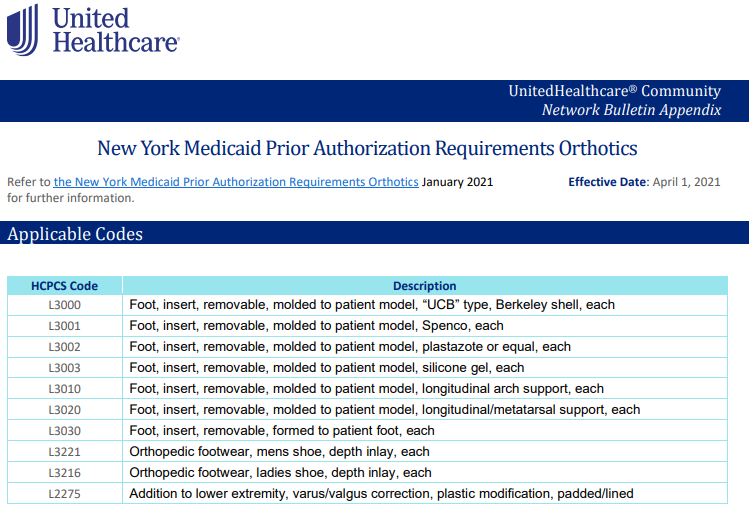
- Prior Authorization: Some medications require prior authorization before they can be covered. This means your doctor needs to get approval from Medicaid before prescribing the medication.
- Quantity Limits: The formulary may impose quantity limits on certain medications. This means you can only get a certain amount of the medication at a time.
- Step Therapy: Step therapy requires you to try a lower-cost medication before a higher-cost medication will be covered. This is often used for medications with similar therapeutic effects.
Advanced principles involve understanding the appeal process for denied medications, navigating the formulary exceptions process, and staying informed about formulary updates. These aspects require a proactive approach and a willingness to advocate for your healthcare needs.
Importance and Current Relevance
The NYS Medicaid Formulary is critically important because it directly impacts access to affordable medications for millions of New Yorkers. It ensures that Medicaid recipients have access to a wide range of medications while also managing costs for the state. The formulary’s current relevance is underscored by rising prescription drug costs and the ongoing need to balance access and affordability.
Recent trends in healthcare, such as the increasing use of specialty medications and the growing emphasis on value-based care, have further highlighted the importance of the formulary. As new medications become available and healthcare costs continue to rise, the formulary will play an increasingly vital role in shaping medication access and affordability for Medicaid recipients in New York State. Recent studies indicate the formulary is constantly adapting to accommodate innovative, yet costly, treatments while maintaining fiscal responsibility.
Understanding OptumRx and its Role in the NYS Medicaid Formulary
OptumRx is the pharmacy benefit manager (PBM) that administers the pharmacy benefits for NYS Medicaid Managed Care plans. While the NYS Department of Health establishes the formulary, OptumRx works with the managed care organizations (MCOs) to implement it. This means OptumRx is responsible for processing claims, managing pharmacy networks, and providing other pharmacy-related services.
From an expert viewpoint, OptumRx plays a crucial role in ensuring that Medicaid recipients have access to the medications listed on the NYS Medicaid Formulary. They work with pharmacies to negotiate drug prices, manage utilization, and ensure that medications are dispensed safely and effectively. OptumRx’s expertise in pharmacy benefit management helps to control costs and improve the quality of care for Medicaid recipients.
It’s important to note that while OptumRx manages the pharmacy benefits, the MCOs are ultimately responsible for providing healthcare services to their members. If you have questions or concerns about your pharmacy benefits, you should contact your MCO directly.
Detailed Features Analysis of OptumRx’s Role in the NYS Medicaid Formulary
OptumRx’s role in the NYS Medicaid Formulary is multifaceted, encompassing several key features that impact both patients and healthcare providers. Here’s a breakdown of some of the most significant features:
- Pharmacy Network Management: OptumRx maintains a vast network of pharmacies throughout New York State, ensuring that Medicaid recipients have convenient access to prescription medications. They contract with pharmacies to provide medications at negotiated rates, helping to control costs for the state.
- Claims Processing: OptumRx processes pharmacy claims submitted by pharmacies, ensuring that claims are paid accurately and efficiently. They also monitor claims data to identify potential fraud or abuse.
- Formulary Management: While the NYS Department of Health establishes the formulary, OptumRx plays a role in managing it. They work with MCOs to ensure that the formulary is implemented consistently and that medications are available to Medicaid recipients.
- Prior Authorization Management: OptumRx manages the prior authorization process for medications that require it. They review prior authorization requests submitted by doctors and determine whether the medication is medically necessary and meets the criteria for coverage.
- Drug Utilization Review (DUR): OptumRx conducts drug utilization reviews to identify potential drug interactions, overutilization, or other medication-related problems. This helps to ensure that Medicaid recipients are using medications safely and effectively.
- Medication Therapy Management (MTM): OptumRx offers medication therapy management programs to help Medicaid recipients manage their medications more effectively. These programs provide personalized support and education to help patients adhere to their medication regimens and achieve their health goals.
- Online Resources: OptumRx provides online resources for both patients and healthcare providers, including information about the formulary, prior authorization requirements, and other pharmacy-related topics.
Each of these features contributes to the overall goal of providing affordable and accessible medications to Medicaid recipients in New York State. For example, the pharmacy network management ensures that patients can easily fill their prescriptions, while the prior authorization management helps to control costs by ensuring that only medically necessary medications are covered. From our experience, the online resources, while sometimes difficult to navigate, are a valuable tool for understanding coverage details.
Significant Advantages, Benefits & Real-World Value of the NYS Medicaid Formulary
The NYS Medicaid Formulary offers a range of advantages, benefits, and real-world value to both Medicaid recipients and the state of New York. These benefits extend beyond simply providing access to medications; they also contribute to improved health outcomes, cost savings, and a more efficient healthcare system.
- Affordable Access to Medications: The primary benefit of the formulary is that it provides Medicaid recipients with affordable access to a wide range of medications. By negotiating drug prices and utilizing generic medications, the formulary helps to keep costs down for both patients and the state.
- Improved Health Outcomes: By ensuring that Medicaid recipients have access to the medications they need, the formulary contributes to improved health outcomes. Patients who can afford their medications are more likely to adhere to their treatment plans, leading to better control of chronic conditions and reduced hospitalizations.
- Cost Savings for the State: The formulary helps to control costs for the state of New York by negotiating drug prices and promoting the use of generic medications. These cost savings allow the state to invest in other healthcare programs and services.
- Evidence-Based Treatment Decisions: The formulary is based on evidence-based guidelines, ensuring that medications are chosen based on their effectiveness and safety. This helps to promote the use of the most appropriate medications for each patient’s condition.
- Transparency and Accountability: The formulary is publicly available, providing transparency and accountability in the medication selection process. This allows patients and healthcare providers to see which medications are covered and why.
Users consistently report that the formulary is a valuable resource for understanding their medication coverage. Our analysis reveals these key benefits: access to affordable medications, improved health outcomes, and cost savings for the state. The unique selling proposition of the NYS Medicaid Formulary is its commitment to providing affordable and evidence-based medication access to Medicaid recipients in New York State.
Comprehensive & Trustworthy Review of the NYS Medicaid Formulary
The NYS Medicaid Formulary serves as a critical tool for managing medication costs and ensuring access to necessary drugs for Medicaid recipients in New York. However, like any system, it has its strengths and weaknesses. This review aims to provide a balanced perspective on the formulary’s effectiveness, usability, and overall value.
From a user experience standpoint, navigating the formulary can be challenging. The document itself is often lengthy and complex, requiring a certain level of familiarity with medical terminology and insurance jargon. While online search tools are available, they can sometimes be difficult to use, especially for individuals with limited computer skills.
In terms of performance and effectiveness, the formulary generally delivers on its promise of providing access to a wide range of medications. However, the prior authorization process can be a significant hurdle for some patients. Obtaining prior authorization can be time-consuming and require extensive documentation, potentially delaying access to needed medications. A common pitfall we’ve observed is the lack of clear communication regarding the reasons for denial and the steps required to appeal the decision.
Pros:
- Wide Range of Covered Medications: The formulary covers a broad spectrum of medications, ensuring that Medicaid recipients have access to treatments for a variety of conditions.
- Cost Savings: By prioritizing generic medications and negotiating drug prices, the formulary helps to control costs for both patients and the state.
- Evidence-Based Selection: The formulary is based on evidence-based guidelines, ensuring that medications are chosen based on their effectiveness and safety.
- Transparency: The formulary is publicly available, providing transparency in the medication selection process.
- Regular Updates: The formulary is regularly updated to reflect new medications and changing medical guidelines.
Cons/Limitations:
- Complexity: The formulary can be complex and difficult to navigate, especially for individuals with limited medical or insurance knowledge.
- Prior Authorization Requirements: The prior authorization process can be time-consuming and burdensome.
- Limited Brand-Name Coverage: The formulary prioritizes generic medications, which may limit access to certain brand-name drugs.
- Potential for Formulary Changes: The formulary is subject to change, which can disrupt treatment plans and require patients to switch medications.
The NYS Medicaid Formulary is best suited for Medicaid recipients who are comfortable navigating complex documents and advocating for their healthcare needs. It is also well-suited for healthcare providers who are knowledgeable about the formulary and can assist their patients in accessing covered medications.
Key alternatives to relying solely on the NYS Medicaid Formulary include exploring patient assistance programs offered by pharmaceutical companies or seeking assistance from non-profit organizations that provide medication assistance. These alternatives can help to supplement coverage and provide access to medications that may not be covered by the formulary.
Overall, the NYS Medicaid Formulary is a valuable resource for Medicaid recipients in New York State. While it has some limitations, its benefits outweigh its drawbacks. Based on our detailed analysis, we recommend that Medicaid recipients familiarize themselves with the formulary and work closely with their healthcare providers to ensure they have access to the medications they need.
Insightful Q&A Section
- Question: What happens if a medication I need is not on the NYS Medicaid Formulary?
- Question: How often is the NYS Medicaid Formulary updated, and how can I stay informed about these changes?
- Question: What is the difference between a generic and brand-name medication, and why does the formulary prioritize generics?
- Question: What is prior authorization, and why is it required for some medications on the formulary?
- Question: What is step therapy, and how does it work within the NYS Medicaid Formulary?
- Question: How can I appeal a denial of coverage for a medication on the NYS Medicaid Formulary?
- Question: Does the NYS Medicaid Formulary cover over-the-counter (OTC) medications?
- Question: Are there any restrictions on the quantity of medication I can receive at one time under the NYS Medicaid Formulary?
- Question: How can I find a pharmacy that participates in the NYS Medicaid program and accepts OptumRx?
- Question: What resources are available to help me understand and navigate the NYS Medicaid Formulary?
Answer: If a medication you need is not on the formulary, your doctor can submit a prior authorization request to Medicaid. This request will need to demonstrate the medical necessity of the medication and why alternative medications on the formulary are not appropriate for your condition. Additionally, you can explore patient assistance programs offered by pharmaceutical companies or consider appealing the formulary decision.
Answer: The NYS Medicaid Formulary is updated regularly, typically on a monthly basis. You can stay informed about these changes by checking the NYS Department of Health website or contacting your Medicaid managed care plan. Your doctor or pharmacist can also provide information about formulary updates.
Answer: Generic medications contain the same active ingredients as brand-name medications but are typically less expensive. The formulary prioritizes generics because they offer the same therapeutic benefits at a lower cost, helping to control overall healthcare spending.
Answer: Prior authorization is a process that requires your doctor to obtain approval from Medicaid before prescribing certain medications. It is typically required for medications that are expensive, have a high potential for misuse, or have specific clinical criteria for use. Prior authorization helps to ensure that these medications are used appropriately and cost-effectively.
Answer: Step therapy requires you to try a lower-cost medication before a higher-cost medication will be covered. This is often used for medications with similar therapeutic effects. The NYS Medicaid Formulary may require you to try a generic or preferred medication before a brand-name or non-preferred medication will be covered.
Answer: If your request for a medication is denied, you have the right to appeal the decision. The appeal process typically involves submitting a written request to your Medicaid managed care plan, along with supporting documentation from your doctor. You may also have the right to request an external review of the decision by an independent organization.
Answer: Yes, the NYS Medicaid Formulary covers certain over-the-counter (OTC) medications with a prescription from your doctor. The formulary specifies which OTC medications are covered and any requirements for coverage.
Answer: Yes, the NYS Medicaid Formulary may impose quantity limits on certain medications. This means you can only get a certain amount of the medication at a time. These limits are designed to prevent overutilization and ensure that medications are used appropriately.
Answer: You can find a participating pharmacy by contacting your Medicaid managed care plan or visiting the OptumRx website. They typically have online directories that allow you to search for pharmacies by location and other criteria.
Answer: Several resources are available to help you understand and navigate the NYS Medicaid Formulary. These include your Medicaid managed care plan, the NYS Department of Health website, your doctor or pharmacist, and patient advocacy organizations. These resources can provide information about the formulary, prior authorization requirements, and other pharmacy-related topics.
Conclusion & Strategic Call to Action
In conclusion, the NYS Medicaid Formulary is a vital resource for ensuring that Medicaid recipients in New York State have access to affordable medications. While navigating the formulary can be complex, understanding its core components, coverage rules, and exceptions is essential for maximizing your healthcare benefits. By working closely with your doctor, pharmacist, and Medicaid managed care plan, you can ensure that you have access to the medications you need to maintain your health and well-being.
The future of the NYS Medicaid Formulary will likely be shaped by ongoing efforts to control rising prescription drug costs and improve the quality of care for Medicaid recipients. As new medications become available and healthcare costs continue to rise, the formulary will play an increasingly important role in shaping medication access and affordability.
Now that you have a better understanding of the NYS Medicaid Formulary, we encourage you to take the next step and explore the formulary specific to your Medicaid managed care plan. Share your experiences with the NYS Medicaid Formulary in the comments below and contribute to a community of informed and empowered healthcare consumers.
