NY Medicaid Drug Formulary: Your Expert Guide to Covered Medications
Navigating the New York Medicaid system can be challenging, especially when it comes to understanding which medications are covered under your plan. The NY Medicaid Drug Formulary, also known as the Preferred Drug List (PDL), is a comprehensive list of medications covered by NY Medicaid. Understanding this formulary is crucial for both patients and healthcare providers to ensure access to necessary treatments while managing costs. This guide provides an in-depth look at the NY Medicaid Drug Formulary, offering clarity and expert insights to help you navigate the system effectively. We aim to provide a resource that demystifies the process, ensuring you can make informed decisions about your healthcare.
Understanding the NY Medicaid Drug Formulary
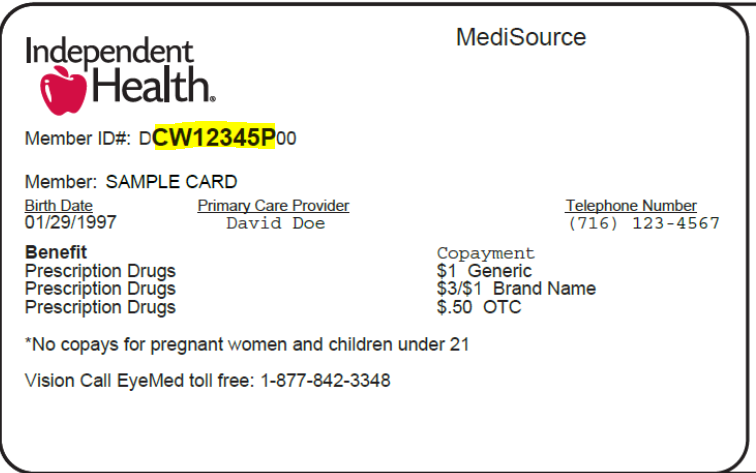
The NY Medicaid Drug Formulary is a continuously updated list of prescription and over-the-counter medications covered by New York State Medicaid. Its primary purpose is to guide prescribers and beneficiaries toward the most effective and cost-efficient medications. The formulary is organized into different tiers, each representing a different cost level for the patient. Understanding the structure and content of the NY Medicaid drug formulary is vital for both healthcare providers and patients.
Core Concepts and Advanced Principles
The formulary isn’t just a list; it’s a complex system designed to balance cost-effectiveness with patient needs. Several key principles underpin its structure:
* **Therapeutic Equivalence:** Medications are often grouped by therapeutic class, and the formulary favors those that are therapeutically equivalent but offer better value.
* **Prior Authorization:** Some medications require prior authorization, meaning your doctor needs to get approval from Medicaid before you can receive the medication. This is often required for more expensive or potentially misused drugs.
* **Step Therapy:** Step therapy requires you to try a lower-cost, first-line treatment before Medicaid will cover a more expensive, second-line treatment. This ensures that simpler, more affordable options are explored first.
* **Quantity Limits:** To prevent overuse or misuse, some medications have quantity limits, restricting the amount you can receive within a given timeframe.
These principles are crucial for understanding how the NY Medicaid drug formulary operates and why certain medications may require additional steps before coverage is approved.
Importance and Current Relevance
The NY Medicaid Drug Formulary plays a critical role in managing healthcare costs for the state while ensuring access to essential medications for its beneficiaries. Its relevance is amplified by the rising cost of prescription drugs and the increasing demand for healthcare services. Recent trends indicate a growing emphasis on value-based care, where the formulary is used as a tool to promote the use of medications that offer the best clinical outcomes at the lowest cost. The formulary is updated frequently to reflect new drug approvals, changes in pricing, and evolving clinical guidelines. Keeping abreast of these changes is essential for healthcare providers and patients alike.
Navigating the eMedNY Website for Formulary Information
The official source for the most up-to-date information on the NY Medicaid Drug Formulary is the eMedNY website. eMedNY is the online portal for New York Medicaid providers, and it offers a wealth of resources, including the complete drug formulary, updates, and related policies. Understanding how to navigate this website is essential for accessing the information you need. Here’s what you need to know:
* **Accessing the Formulary:** The formulary is typically available as a downloadable PDF document or as a searchable online database. The eMedNY website provides clear instructions on how to access both.
* **Searching for Medications:** The online database allows you to search for medications by name, generic name, or therapeutic class. This makes it easy to find specific information about a drug’s coverage status.
* **Understanding Formulary Tiers:** The formulary categorizes drugs into different tiers, each with its own cost-sharing requirements. Understanding these tiers is crucial for estimating your out-of-pocket expenses.
* **Finding Updates and Changes:** The eMedNY website regularly publishes updates and changes to the formulary. It’s important to check these updates frequently to stay informed about any changes that may affect your coverage.
Detailed Features Analysis of the NY Medicaid Drug Formulary
The NY Medicaid Drug Formulary is more than just a list of covered drugs; it’s a complex system with several key features designed to optimize medication use and control costs. Here’s a detailed breakdown of some of its most important features:
1. **Tiered Structure:** Medications are categorized into different tiers, each with its own cost-sharing requirements. Typically, lower tiers include generic drugs with lower co-pays, while higher tiers include brand-name drugs with higher co-pays. This encourages the use of more cost-effective medications.
2. **Preferred Drug List (PDL):** The PDL highlights preferred medications within each therapeutic class. These are typically the most cost-effective options that are still clinically effective. Prescribers are encouraged to prescribe medications from the PDL whenever possible.
3. **Prior Authorization (PA):** Certain medications require prior authorization before they can be covered. This is often required for drugs that are expensive, have a high potential for misuse, or require close monitoring.
4. **Step Therapy (ST):** Step therapy requires patients to try a lower-cost, first-line medication before Medicaid will cover a more expensive, second-line medication. This ensures that simpler, more affordable options are explored first.
5. **Quantity Limits (QL):** To prevent overuse or misuse, some medications have quantity limits, restricting the amount you can receive within a given timeframe.
6. **Non-Preferred Drug List:** This list details medications that are not preferred and may require prior authorization or have higher co-pays. It’s important to be aware of this list to understand which medications may be more difficult to access.
7. **Updates and Revisions:** The formulary is regularly updated to reflect new drug approvals, changes in pricing, and evolving clinical guidelines. These updates are essential for healthcare providers and patients to stay informed about any changes that may affect coverage.
Each of these features plays a crucial role in managing the NY Medicaid Drug Formulary and ensuring that beneficiaries have access to the medications they need while controlling costs.
Significant Advantages, Benefits & Real-World Value of the NY Medicaid Drug Formulary
The NY Medicaid Drug Formulary offers several advantages and benefits that directly impact both patients and the healthcare system. Here’s a look at the real-world value it provides:
* **Cost Savings:** By favoring generic and preferred drugs, the formulary helps to lower overall healthcare costs for both Medicaid and its beneficiaries. This allows Medicaid to allocate resources more efficiently and ensures that patients can afford their medications.
* **Access to Essential Medications:** The formulary ensures that beneficiaries have access to a wide range of essential medications. While some drugs may require prior authorization or step therapy, the formulary ultimately aims to provide access to the treatments patients need.
* **Improved Medication Management:** The formulary encourages the use of evidence-based guidelines and best practices for medication management. This helps to ensure that patients receive the most appropriate and effective treatments.
* **Transparency and Information:** The eMedNY website provides a wealth of information about the formulary, including drug lists, updates, and policies. This transparency empowers patients and healthcare providers to make informed decisions about medication use.
* **Promoting Generic Drug Use:** The formulary actively promotes the use of generic drugs, which are typically much more affordable than brand-name drugs. This helps to lower costs without sacrificing quality or effectiveness.
* **Standardized Treatment Protocols:** By guiding prescribers toward preferred medications, the formulary helps to standardize treatment protocols and reduce variations in care. This can lead to better outcomes for patients.
* **Efficient Resource Allocation:** By managing drug costs effectively, the formulary allows Medicaid to allocate resources to other important healthcare services, such as preventative care and mental health services.
Comprehensive & Trustworthy Review of the NY Medicaid Drug Formulary
The NY Medicaid Drug Formulary is a vital component of the state’s healthcare system, designed to provide affordable access to necessary medications for eligible residents. However, like any complex system, it has its strengths and weaknesses.
**User Experience & Usability:**
Navigating the eMedNY website, the primary source of information on the formulary, can be challenging for some users. While the website provides a wealth of information, it can be overwhelming and difficult to navigate, especially for those who are not familiar with the Medicaid system. A more user-friendly interface and clearer instructions would greatly improve the user experience.
**Performance & Effectiveness:**
The formulary is generally effective in controlling drug costs and promoting the use of generic medications. However, the prior authorization and step therapy requirements can sometimes create barriers to access, particularly for patients with complex medical conditions. Streamlining these processes and providing more flexibility for individual cases would improve the system’s effectiveness.
**Pros:**
1. **Cost Control:** The formulary effectively manages drug costs by favoring generic and preferred medications.
2. **Access to Essential Medications:** It ensures access to a wide range of essential medications for Medicaid beneficiaries.
3. **Promotes Generic Drug Use:** It actively encourages the use of generic drugs, which are more affordable.
4. **Transparency:** The eMedNY website provides a wealth of information about the formulary.
5. **Regular Updates:** The formulary is regularly updated to reflect new drug approvals and changes in pricing.
**Cons/Limitations:**
1. **Prior Authorization Requirements:** The prior authorization process can be cumbersome and time-consuming.
2. **Step Therapy Requirements:** Step therapy can delay access to the most appropriate medication for some patients.
3. **Website Usability:** The eMedNY website can be difficult to navigate for some users.
4. **Limited Coverage for Some Medications:** Some medications may not be covered or may have limited coverage.
**Ideal User Profile:**
The NY Medicaid Drug Formulary is best suited for individuals who are eligible for Medicaid in New York State and who require prescription medications. It is particularly beneficial for those who are willing to use generic medications and who are able to navigate the prior authorization and step therapy requirements.
**Key Alternatives (Briefly):**
Other insurance plans, such as Medicare Part D or private insurance, may offer different formularies and coverage options. However, these plans typically have higher premiums and co-pays than Medicaid.
**Expert Overall Verdict & Recommendation:**
The NY Medicaid Drug Formulary is a valuable resource for ensuring access to affordable medications for eligible New Yorkers. While it has some limitations, its benefits outweigh its drawbacks. We recommend that patients and healthcare providers familiarize themselves with the formulary and work together to navigate the system effectively. Streamlining the prior authorization and step therapy processes and improving the usability of the eMedNY website would further enhance the formulary’s effectiveness.
Insightful Q&A Section
Here are 10 insightful questions and answers related to the NY Medicaid Drug Formulary, addressing common user pain points and advanced queries:
1. **Question:** How often is the NY Medicaid Drug Formulary updated, and where can I find the most recent version?
**Answer:** The NY Medicaid Drug Formulary is updated regularly, typically on a monthly basis. The most recent version can be found on the eMedNY website under the “Pharmacy” section. Be sure to check the update date to ensure you have the latest information.
2. **Question:** What is the difference between a preferred and non-preferred drug on the formulary, and how does it affect my co-pay?
**Answer:** A preferred drug is a medication that is favored by the formulary due to its cost-effectiveness and clinical efficacy. Non-preferred drugs are typically more expensive or have less favorable clinical profiles. Preferred drugs usually have lower co-pays than non-preferred drugs.
3. **Question:** What is prior authorization, and how do I know if my medication requires it?
**Answer:** Prior authorization is a process where your doctor needs to get approval from Medicaid before you can receive a particular medication. This is often required for drugs that are expensive, have a high potential for misuse, or require close monitoring. The formulary will indicate which medications require prior authorization.
4. **Question:** What is step therapy, and how does it work within the NY Medicaid system?
**Answer:** Step therapy requires you to try a lower-cost, first-line treatment before Medicaid will cover a more expensive, second-line treatment. This ensures that simpler, more affordable options are explored first. Your doctor will need to document that the first-line treatment was ineffective before you can move on to the second-line treatment.
5. **Question:** What happens if a medication I need is not on the NY Medicaid Drug Formulary?
**Answer:** If a medication you need is not on the formulary, your doctor can submit a request for a formulary exception. This requires your doctor to provide documentation supporting the medical necessity of the medication.
6. **Question:** How can I find out the co-pay for a specific medication on the NY Medicaid Drug Formulary?
**Answer:** Co-pay information is typically available on the eMedNY website or by contacting your Medicaid managed care plan. Co-pays vary depending on the drug tier and your specific plan.
7. **Question:** Are there any over-the-counter medications covered by the NY Medicaid Drug Formulary?
**Answer:** Yes, some over-the-counter medications are covered by the formulary with a prescription from your doctor. Check the formulary for a list of covered over-the-counter medications.
8. **Question:** What should I do if my prior authorization request is denied?
**Answer:** If your prior authorization request is denied, you have the right to appeal the decision. Your doctor can assist you with the appeals process.
9. **Question:** How does the NY Medicaid Drug Formulary handle specialty medications, such as those for chronic conditions like HIV or hepatitis C?
**Answer:** Specialty medications are often covered by the formulary, but they may require prior authorization and have specific dispensing requirements. Your doctor can provide more information about accessing specialty medications.
10. **Question:** Can I switch between different Medicaid managed care plans if I am not satisfied with the drug coverage offered by my current plan?
**Answer:** Yes, you typically have the option to switch between Medicaid managed care plans during open enrollment periods or under certain circumstances. Compare the drug coverage offered by different plans before making a decision.
Conclusion & Strategic Call to Action
Understanding the NY Medicaid Drug Formulary is essential for accessing affordable medications and navigating the complexities of the New York Medicaid system. This guide has provided a comprehensive overview of the formulary, its key features, and its real-world value. By understanding how the formulary works, you can make informed decisions about your healthcare and ensure that you have access to the medications you need. The NY Medicaid Drug Formulary is a complex but vital tool for managing healthcare costs and ensuring access to essential medications for eligible New Yorkers. While navigating the system can be challenging, understanding its core principles and features is crucial for both patients and healthcare providers.
For further information and assistance, explore the eMedNY website or contact your Medicaid managed care plan. Share your experiences with the NY Medicaid Drug Formulary in the comments below to help others navigate the system effectively.
