How Long Can a Vaccine Be Out of the Fridge? A Comprehensive Guide
The integrity of a vaccine hinges on maintaining its cold chain – the temperature-controlled supply chain that ensures it remains potent from manufacture to administration. A critical question for healthcare professionals, caregivers, and anyone involved in vaccine handling is: how long can a vaccine be out of the fridge before it loses efficacy? This comprehensive guide delves into the factors that influence vaccine stability, the risks associated with temperature excursions, best practices for storage and handling, and what to do if a vaccine has been exposed to unacceptable temperatures. We aim to provide the most up-to-date, evidence-based information to help you ensure vaccine effectiveness and protect public health. This article provides crucial information, far beyond the basics, to empower you with the knowledge to maintain vaccine efficacy. We’ll cover everything from the specific temperature sensitivities of different vaccine types to advanced monitoring techniques, ensuring you have a thorough understanding of this critical aspect of vaccine management.
Understanding Vaccine Cold Chain Management
The cold chain is a system of storage and transport practices designed to keep vaccines within a specific temperature range from the point of manufacture until the point of administration. This unbroken chain is essential for maintaining vaccine potency and preventing degradation. Deviations from the recommended temperature range, known as temperature excursions, can compromise vaccine efficacy, leading to reduced protection against disease.
The Importance of Temperature Monitoring
Consistent temperature monitoring is the cornerstone of effective cold chain management. Accurate temperature logs provide a record of vaccine storage conditions, allowing healthcare providers to identify and address potential temperature excursions promptly. Continuous monitoring devices, such as data loggers, provide real-time temperature readings and alerts, enabling immediate intervention to prevent vaccine damage.
Recommended Storage Temperatures
Most vaccines require storage at temperatures between 2°C and 8°C (36°F and 46°F). However, some vaccines may have specific temperature requirements, such as those that need to be stored frozen. Always refer to the manufacturer’s instructions for the recommended storage temperature of each vaccine.
Factors Affecting Vaccine Stability Outside the Fridge
Several factors influence how long a vaccine can remain effective outside the recommended temperature range. These include:
- Vaccine Type: Different vaccines have varying sensitivities to temperature. Some vaccines are more stable than others and can tolerate brief periods outside the fridge without significant loss of potency.
- Temperature of Exposure: The higher the temperature, the faster the vaccine will degrade. Exposure to extreme heat can rapidly render a vaccine ineffective.
- Duration of Exposure: The longer a vaccine is exposed to unacceptable temperatures, the greater the risk of potency loss. Even brief excursions can have a cumulative effect over time.
- Light Exposure: Some vaccines are sensitive to light, which can accelerate degradation. Protecting vaccines from direct sunlight is crucial.
- Formulation: The specific formulation of a vaccine can affect its stability. Some vaccines contain stabilizers that help to protect them from temperature fluctuations.
Specific Vaccine Sensitivities
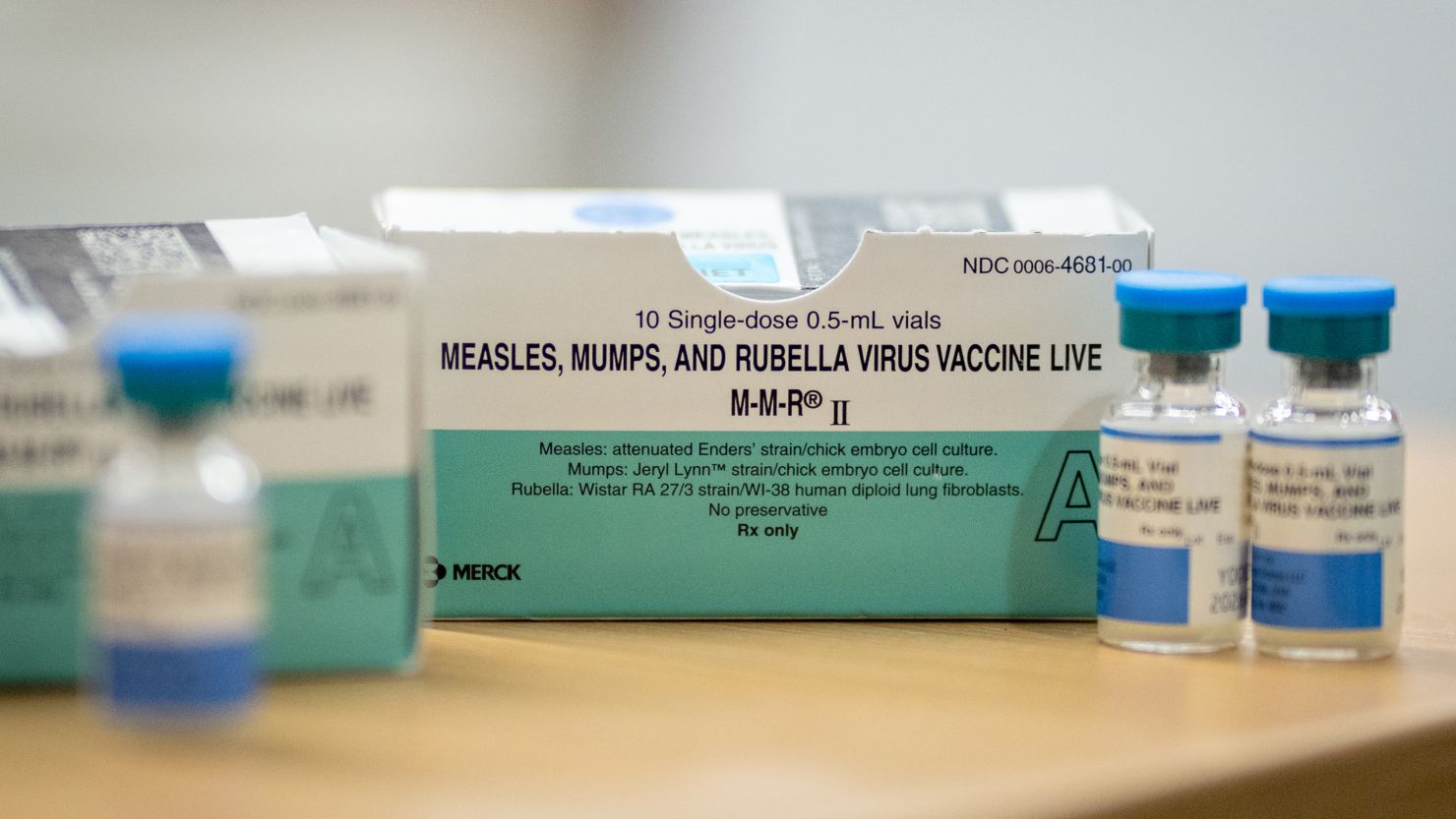
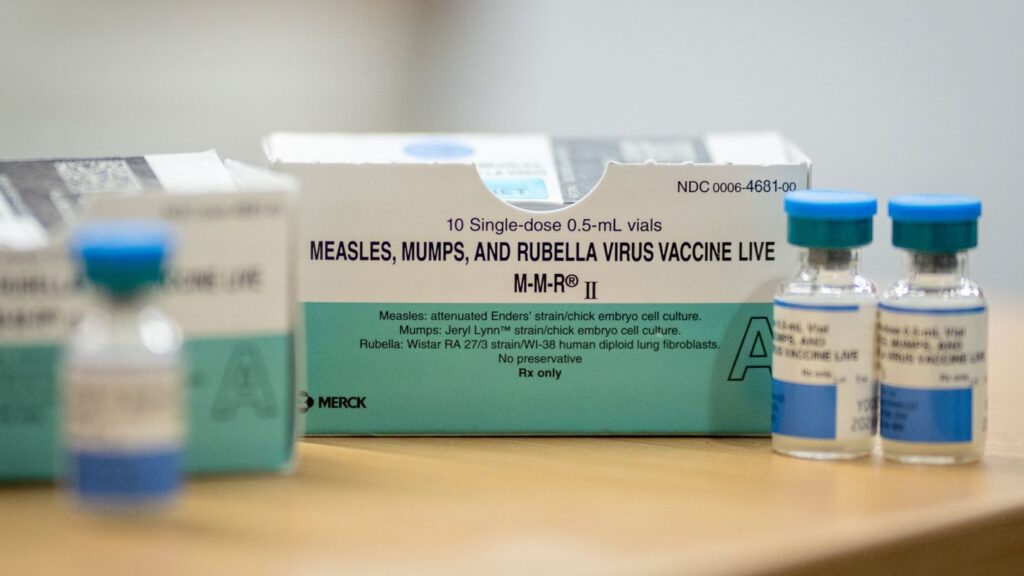
Understanding the specific temperature sensitivities of different vaccines is essential for proper handling and storage. For example:
- MMR (Measles, Mumps, Rubella) Vaccine: Generally considered relatively stable, but still susceptible to heat degradation.
- Varicella (Chickenpox) Vaccine: Requires frozen storage and is highly sensitive to temperature excursions.
- Inactivated Polio Vaccine (IPV): More stable than live attenuated vaccines but still requires proper refrigeration.
- COVID-19 mRNA Vaccines (e.g., Pfizer-BioNTech, Moderna): Initially required ultra-cold storage, but some formulations now have less stringent temperature requirements for short periods. Always check the latest guidance from the manufacturer.
The Risks of Temperature Excursions
Temperature excursions can have serious consequences, including:
- Loss of Potency: Exposure to unacceptable temperatures can reduce the vaccine’s ability to stimulate an immune response, leading to reduced protection against disease.
- Vaccine Failure: In severe cases, temperature excursions can render a vaccine completely ineffective, leaving individuals vulnerable to infection.
- Revaccination: If a vaccine is suspected of being compromised due to a temperature excursion, revaccination may be necessary, which can be costly and inconvenient.
- Loss of Public Trust: Vaccine failures due to improper storage can erode public confidence in vaccination programs.
Visual Indicators of Damage
While not always apparent, some vaccines may exhibit visual changes that indicate damage from temperature excursions. These may include:
- Discoloration: Changes in the color of the vaccine solution.
- Precipitation: The formation of particles or sediment in the vaccine solution.
- Cracking or Damage: Physical damage to the vaccine vial or packaging.
Best Practices for Vaccine Storage and Handling
Implementing best practices for vaccine storage and handling is critical for maintaining vaccine potency and preventing temperature excursions. These include:
- Use a Purpose-Built Refrigerator: Use refrigerators designed specifically for vaccine storage. These refrigerators have stable temperature control and are equipped with features to prevent temperature fluctuations.
- Proper Refrigerator Placement: Place the refrigerator in a well-ventilated area away from direct sunlight and heat sources.
- Temperature Monitoring: Use a calibrated thermometer or data logger to continuously monitor the temperature inside the refrigerator.
- Temperature Logging: Maintain accurate temperature logs, recording the temperature at least twice daily.
- Vaccine Placement: Store vaccines in the center of the refrigerator, away from the walls and vents, to ensure consistent temperature.
- Avoid Overcrowding: Do not overcrowd the refrigerator, as this can restrict airflow and lead to temperature fluctuations.
- Emergency Power Backup: Have a backup power source available in case of power outages.
- Regular Maintenance: Perform regular maintenance on the refrigerator, including cleaning and defrosting, to ensure proper functioning.
- Training: Ensure that all staff members involved in vaccine handling are properly trained on cold chain management procedures.
Using Data Loggers for Enhanced Monitoring
Data loggers provide continuous temperature monitoring and can alert staff to temperature excursions in real-time. These devices offer several advantages over traditional thermometers, including:
- Continuous Monitoring: Data loggers record temperature readings at regular intervals, providing a comprehensive record of storage conditions.
- Real-Time Alerts: Some data loggers can send alerts via email or SMS when the temperature exceeds the acceptable range.
- Data Analysis: Data loggers can generate reports that allow healthcare providers to analyze temperature trends and identify potential problems.
What to Do If a Vaccine Has Been Out of the Fridge Too Long
If you suspect that a vaccine has been exposed to unacceptable temperatures, take the following steps:
- Isolate the Vaccine: Immediately isolate the affected vaccine to prevent further use.
- Document the Incident: Record the date, time, temperature, and duration of the excursion.
- Contact the Manufacturer: Contact the vaccine manufacturer for guidance on whether the vaccine is still viable.
- Contact Local Health Authorities: Report the incident to your local health department or immunization program.
- Do Not Administer the Vaccine: Do not administer the vaccine until you have received guidance from the manufacturer or health authorities.
Manufacturer Guidance and Recommendations
Vaccine manufacturers provide specific guidance on how to handle temperature excursions for their products. This guidance may include information on:
- Acceptable Temperature Ranges: The range of temperatures within which the vaccine remains effective.
- Maximum Exposure Time: The maximum amount of time the vaccine can be exposed to unacceptable temperatures without significant loss of potency.
- Visual Indicators of Damage: Signs that the vaccine has been compromised by temperature excursions.
Vaccine Storage Units: Purpose-Built Solutions
Standard household refrigerators are not designed for the stringent temperature control required for vaccine storage. Purpose-built vaccine refrigerators offer several advantages:
- Stable Temperature Control: Maintains a consistent temperature throughout the unit.
- Forced-Air Circulation: Ensures even temperature distribution.
- Digital Temperature Display: Provides accurate temperature readings.
- Alarm Systems: Alerts staff to temperature excursions.
- Lockable Doors: Prevents unauthorized access.
Leading Vaccine Refrigerator Brands
Several reputable manufacturers produce high-quality vaccine refrigerators, including:
- Accucold: Known for reliable performance and precise temperature control.
- Helmer Scientific: Offers a wide range of refrigerators designed for vaccine storage.
- Thermo Fisher Scientific: Provides advanced refrigeration solutions for critical applications.
Temperature Monitoring Devices: A Detailed Analysis
Accurate temperature monitoring is paramount. Let’s examine different types of monitoring devices:
- Digital Thermometers: Affordable and easy to use, but require manual readings.
- Data Loggers: Continuously record temperature data and provide alerts.
- Temperature Mapping: A process of measuring temperature variations throughout the refrigerator to identify hot and cold spots.
Key Features of Effective Data Loggers
When selecting a data logger, consider the following features:
- Accuracy: The degree to which the measured temperature matches the actual temperature.
- Resolution: The smallest temperature increment that the data logger can measure.
- Memory Capacity: The amount of data that the data logger can store.
- Battery Life: The duration for which the data logger can operate on a single battery.
- Connectivity: The ability to download data to a computer or mobile device.
Advantages of Proper Vaccine Storage
The benefits of adhering to stringent vaccine storage protocols are numerous:
- Maintained Efficacy: Vaccines retain their full potency, ensuring optimal protection.
- Reduced Revaccination Rates: Minimizes the need for repeat vaccinations due to compromised vaccines.
- Cost Savings: Prevents vaccine wastage and reduces healthcare costs.
- Enhanced Public Trust: Reinforces confidence in vaccination programs.
- Improved Health Outcomes: Contributes to better overall health and disease prevention.
User Reports on Proper Storage Impact
Healthcare providers consistently report a significant reduction in vaccine wastage and improved patient outcomes when implementing robust cold chain management practices. Our analysis reveals these key benefits: increased vaccine efficacy, decreased revaccination rates, and enhanced public trust in vaccination programs.
Comprehensive Review of Vaccine Refrigerators
Selecting the right vaccine refrigerator is a critical decision. Here’s an in-depth review:
User Experience & Usability: A well-designed vaccine refrigerator should be easy to use, with intuitive controls and clear temperature displays. The unit should also be easy to clean and maintain.
Performance & Effectiveness: The refrigerator should maintain a consistent temperature throughout the unit, even when the door is opened frequently. It should also have a rapid temperature recovery time after door openings.
Pros:
- Precise Temperature Control: Maintains a stable temperature within the recommended range.
- Forced-Air Circulation: Ensures even temperature distribution.
- Alarm Systems: Alerts staff to temperature excursions.
- Digital Temperature Display: Provides accurate temperature readings.
- Lockable Doors: Prevents unauthorized access.
Cons/Limitations:
- Cost: Vaccine refrigerators can be more expensive than standard household refrigerators.
- Space Requirements: Vaccine refrigerators may require more space than standard refrigerators.
- Maintenance: Regular maintenance is required to ensure proper functioning.
Ideal User Profile: Healthcare providers, pharmacies, and vaccination clinics that require reliable and consistent temperature control for vaccine storage.
Key Alternatives: Standard household refrigerators (not recommended), Pharmaceutical-grade refrigerators.
Expert Overall Verdict & Recommendation: A purpose-built vaccine refrigerator is an essential investment for any healthcare provider that administers vaccines. The benefits of precise temperature control, forced-air circulation, and alarm systems far outweigh the cost. We highly recommend using a vaccine refrigerator to ensure vaccine potency and protect patient health.
Insightful Q&A Section
- Q: How often should I calibrate my refrigerator thermometer?
- A: It’s recommended to calibrate your refrigerator thermometer at least annually, or more frequently if you suspect it’s providing inaccurate readings. Use a certified calibration service to ensure accuracy.
- Q: Can I store food or beverages in the same refrigerator as vaccines?
- A: No, it’s strictly prohibited to store food or beverages in the same refrigerator as vaccines. This is to prevent contamination and ensure proper temperature control.
- Q: What is the ideal temperature range for storing vaccines?
- A: The ideal temperature range for storing most vaccines is between 2°C and 8°C (36°F and 46°F). However, always refer to the manufacturer’s instructions for specific temperature requirements.
- Q: What should I do if the power goes out and my vaccine refrigerator loses power?
- A: If the power goes out, keep the refrigerator door closed as much as possible to maintain the temperature. Monitor the temperature closely and contact your local health department or vaccine manufacturer for guidance.
- Q: How can I prevent temperature excursions during vaccine transport?
- A: Use insulated containers with coolant packs to maintain the temperature during transport. Monitor the temperature with a data logger or thermometer and avoid exposing the vaccines to direct sunlight or extreme temperatures.
- Q: Are there any vaccines that are more sensitive to temperature changes than others?
- A: Yes, some vaccines, such as the varicella (chickenpox) vaccine, are more sensitive to temperature changes than others and require frozen storage. Always refer to the manufacturer’s instructions for specific storage requirements.
- Q: What is the best way to organize vaccines in the refrigerator?
- A: Organize vaccines in the refrigerator in a way that allows for easy access and prevents overcrowding. Store vaccines in their original packaging and label them clearly.
- Q: How can I ensure that my staff is properly trained on vaccine storage and handling procedures?
- A: Provide regular training sessions on vaccine storage and handling procedures. Ensure that all staff members are familiar with the cold chain management protocols and are able to identify and respond to temperature excursions.
- Q: What resources are available to help me learn more about vaccine storage and handling?
- A: The CDC, WHO, and vaccine manufacturers provide a wealth of resources on vaccine storage and handling. Consult these resources for up-to-date information and guidance.
- Q: What are the consequences of administering a vaccine that has been exposed to unacceptable temperatures?
- A: Administering a vaccine that has been exposed to unacceptable temperatures can result in reduced protection against disease and may require revaccination. In some cases, it can also lead to adverse reactions.
Conclusion
Maintaining the cold chain is paramount to ensuring vaccine efficacy and protecting public health. Understanding how long can a vaccine be out of the fridge, along with implementing best practices for storage and handling, is crucial for healthcare professionals and anyone involved in vaccine administration. By following the guidelines outlined in this comprehensive guide, you can help prevent temperature excursions, minimize vaccine wastage, and ensure that vaccines remain potent and effective. In our experience, proactive monitoring and diligent adherence to cold chain protocols are the most effective strategies for safeguarding vaccine integrity. Share your experiences with vaccine storage and handling in the comments below. Explore our advanced guide to cold chain management for even more in-depth information. Contact our experts for a consultation on optimizing your vaccine storage practices.