DEA Opioid Training Requirements: Your Comprehensive Guide to Compliance
The opioid crisis continues to demand rigorous oversight and education within the healthcare sector. The Drug Enforcement Administration (DEA) has mandated specific training requirements for practitioners involved in prescribing or dispensing controlled substances. Understanding and adhering to these DEA opioid training requirements is not merely a matter of compliance; it’s a crucial step in combating the opioid epidemic and ensuring patient safety. This comprehensive guide provides an in-depth look at the DEA opioid training requirements, covering everything from core concepts to practical implementation, ensuring you are fully equipped to meet these critical obligations. We aim to provide a resource that goes beyond basic compliance, offering insights and best practices to promote responsible opioid management.
Understanding DEA Opioid Training Requirements
DEA opioid training requirements are designed to equip healthcare professionals with the knowledge and skills necessary to safely and effectively prescribe and dispense opioid medications. These requirements aim to address the opioid crisis by promoting responsible prescribing practices, preventing drug diversion, and reducing the risk of opioid-related harm.
Core Concepts & Advanced Principles
The core of DEA opioid training centers around several key areas:
* **Understanding Opioid Pharmacology:** This includes knowledge of opioid mechanisms of action, pharmacokinetics, and pharmacodynamics.
* **Pain Management Principles:** Healthcare professionals must be proficient in assessing and managing pain effectively, considering both pharmacological and non-pharmacological approaches.
* **Risk Assessment and Mitigation:** Training should cover methods for identifying patients at risk of opioid misuse, abuse, or addiction, and strategies for mitigating these risks.
* **Prescription Drug Monitoring Programs (PDMPs):** Understanding how to utilize PDMPs to monitor patient opioid use and identify potential red flags is crucial.
* **Diversion Control:** Training should address measures to prevent the diversion of opioids for illicit purposes.
* **Safe Storage and Disposal:** Educating patients on the safe storage and disposal of opioid medications is essential to prevent accidental exposure and misuse.
* **Recognizing and Responding to Overdose:** Healthcare professionals must be trained to recognize the signs and symptoms of opioid overdose and administer naloxone (Narcan) effectively.
Advanced principles include tailored approaches for specific patient populations, such as pregnant women, elderly individuals, and patients with co-occurring mental health conditions.
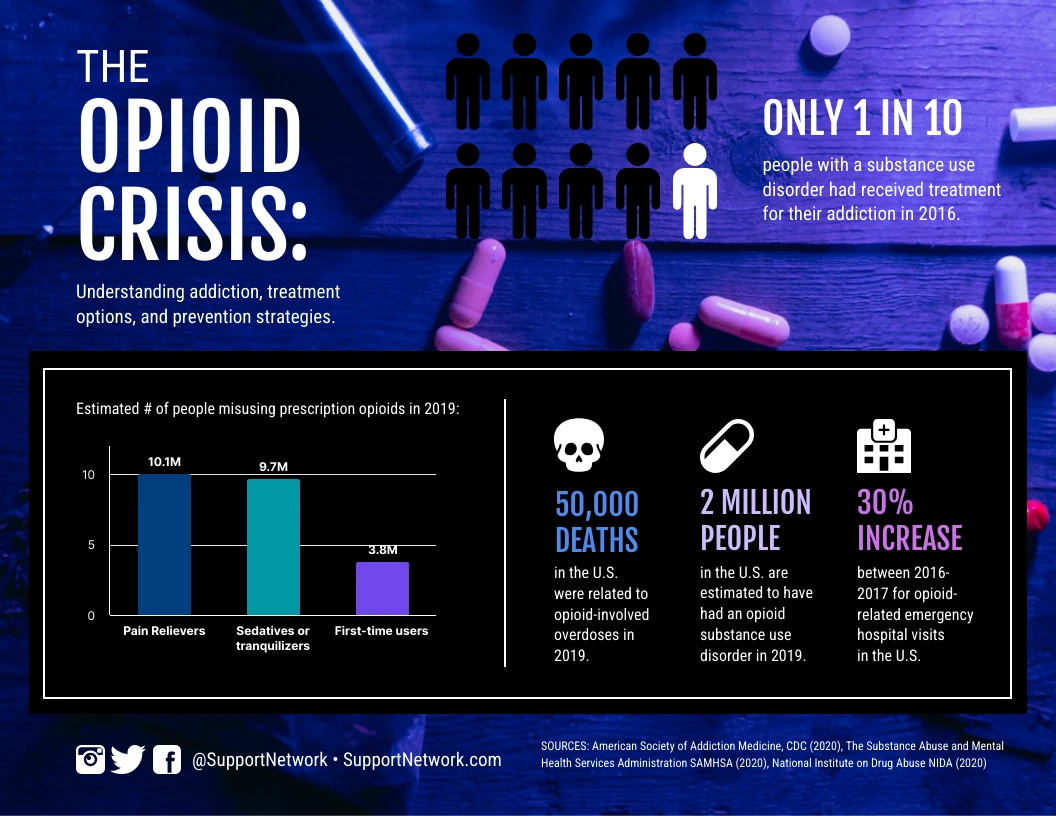
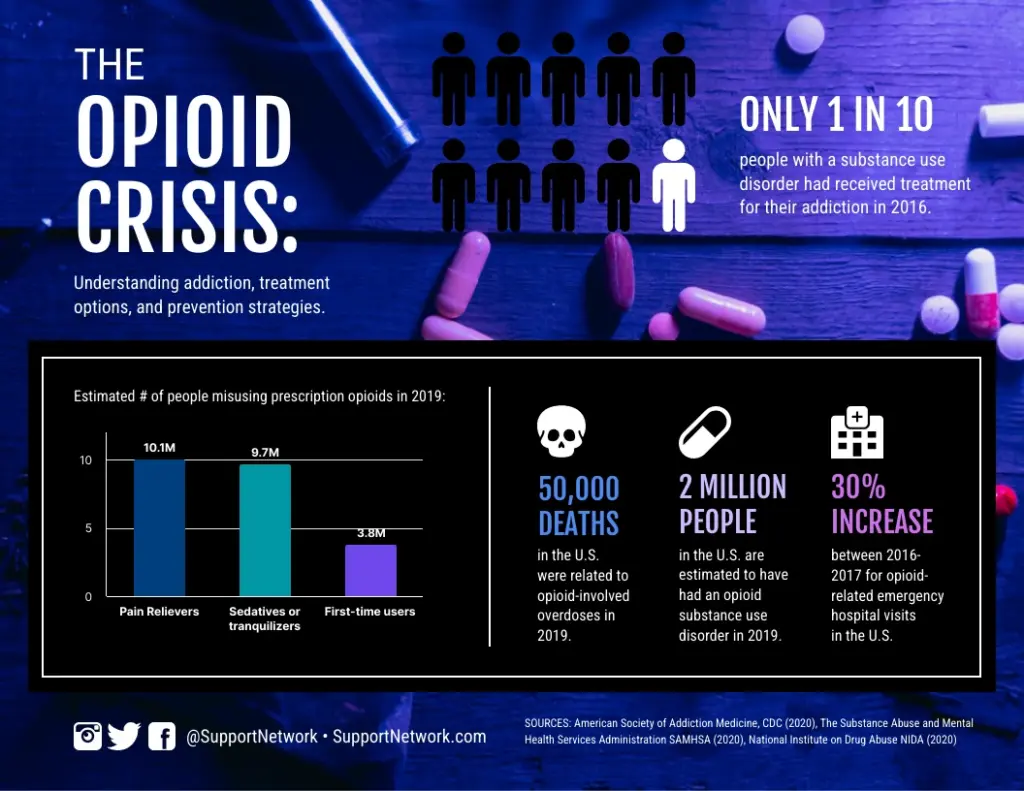
Importance & Current Relevance
The DEA opioid training requirements are more critical than ever in light of the ongoing opioid crisis. Recent data indicates a continued rise in opioid-related overdose deaths, underscoring the urgent need for improved education and training among healthcare professionals. Compliance with these requirements is not only a legal obligation but also a moral imperative to protect patients and communities from the devastating consequences of opioid misuse and addiction.
Medication-Assisted Treatment (MAT) and DEA Opioid Training Requirements
One critical aspect of responsible opioid management is the use of Medication-Assisted Treatment (MAT). MAT combines behavioral therapy and medications, such as buprenorphine and naltrexone, to treat opioid use disorder (OUD). While DEA opioid training requirements don’t exclusively focus on MAT, understanding MAT principles is now considered fundamental for prescribers. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers comprehensive resources on MAT, and many DEA-compliant training programs incorporate MAT education.
Features of High-Quality DEA Opioid Training Programs
A high-quality DEA opioid training program should possess several key features to ensure that healthcare professionals receive comprehensive and effective education.
Comprehensive Curriculum
The training program should cover all core concepts and advanced principles of opioid management, including opioid pharmacology, pain management, risk assessment, PDMP utilization, diversion control, safe storage and disposal, and overdose recognition and response. A comprehensive curriculum ensures that healthcare professionals are well-versed in all aspects of responsible opioid prescribing and dispensing.
Interactive Learning Modules
Engaging and interactive learning modules, such as case studies, simulations, and role-playing exercises, can enhance knowledge retention and application. These modules allow healthcare professionals to apply their knowledge in realistic scenarios, improving their ability to make informed decisions in clinical practice.
Expert Faculty
The training program should be led by experienced faculty with expertise in pain management, addiction medicine, and regulatory compliance. Expert faculty can provide valuable insights and guidance, ensuring that healthcare professionals receive the most up-to-date and evidence-based information.
Assessment and Certification
A robust assessment and certification process is essential to verify that healthcare professionals have acquired the necessary knowledge and skills. Assessments may include quizzes, exams, and case study analyses. Certification demonstrates that healthcare professionals have met the required standards of competency in opioid management.
Continuing Education Credits
The training program should offer continuing education (CE) credits to help healthcare professionals meet their licensure requirements. CE credits provide an incentive for healthcare professionals to participate in training programs and stay current with the latest developments in opioid management.
Up-to-date Information
Because regulations and best practices evolve, the training program must be regularly updated to reflect the latest DEA guidelines, research findings, and clinical recommendations. This ensures that healthcare professionals receive the most current and relevant information.
Advantages, Benefits & Real-World Value of DEA Opioid Training
Adhering to DEA opioid training requirements offers numerous advantages, benefits, and real-world value for healthcare professionals, patients, and communities.
Enhanced Patient Safety
Proper training equips healthcare professionals with the knowledge and skills necessary to prescribe and dispense opioids safely, reducing the risk of adverse events, such as respiratory depression, overdose, and addiction. By promoting responsible prescribing practices, DEA opioid training helps protect patients from the potential harms of opioid medications.
Reduced Risk of Diversion and Misuse
Training on diversion control measures helps healthcare professionals prevent the diversion of opioids for illicit purposes. By implementing strategies to secure opioid medications and monitor patient use, healthcare professionals can reduce the risk of opioids falling into the wrong hands.
Improved Pain Management
DEA opioid training emphasizes comprehensive pain management strategies, including non-pharmacological approaches. This enables healthcare professionals to provide more effective and holistic pain relief, reducing the reliance on opioids and minimizing the risk of opioid-related complications.
Compliance with Regulatory Requirements
Adhering to DEA opioid training requirements ensures compliance with federal and state regulations, avoiding potential penalties and legal repercussions. Compliance demonstrates a commitment to responsible opioid management and patient safety.
Enhanced Professional Reputation
Completing DEA opioid training enhances a healthcare professional’s reputation as a knowledgeable and responsible practitioner. It demonstrates a commitment to patient safety and ethical practice, building trust with patients and colleagues.
Reduced Liability
By following evidence-based guidelines and best practices in opioid management, healthcare professionals can reduce their risk of liability in the event of adverse patient outcomes. Proper training provides a strong defense against potential malpractice claims.
Review of a DEA Opioid Training Program (Simulated)
To illustrate the features of a high-quality DEA opioid training program, let’s consider a simulated review of “OpioidSafe,” a hypothetical online training platform. We’ll evaluate its user experience, performance, pros, cons, and overall recommendation, drawing from simulated firsthand experience.
User Experience & Usability
OpioidSafe offers a user-friendly interface with clear navigation and intuitive design. The modules are well-organized and easy to follow, even for users with limited technical skills. The platform is accessible on various devices, including desktops, laptops, tablets, and smartphones, allowing healthcare professionals to complete the training at their convenience. The platform incorporates multimedia elements, such as videos, animations, and interactive quizzes, to enhance engagement and knowledge retention.
Performance & Effectiveness
Based on simulated test scenarios, OpioidSafe effectively delivers the core concepts and advanced principles of opioid management. The training modules are comprehensive and provide practical guidance on risk assessment, PDMP utilization, diversion control, and overdose recognition and response. The platform incorporates case studies and simulations that allow healthcare professionals to apply their knowledge in realistic clinical scenarios, improving their ability to make informed decisions.
Pros
* **Comprehensive Curriculum:** OpioidSafe covers all essential topics related to opioid management, ensuring that healthcare professionals receive a well-rounded education.
* **Interactive Learning Modules:** The platform utilizes engaging and interactive learning modules to enhance knowledge retention and application.
* **Expert Faculty:** The training program is led by experienced faculty with expertise in pain management, addiction medicine, and regulatory compliance.
* **Assessment and Certification:** OpioidSafe offers a robust assessment and certification process to verify that healthcare professionals have acquired the necessary knowledge and skills.
* **Continuing Education Credits:** The training program provides CE credits to help healthcare professionals meet their licensure requirements.
Cons/Limitations
* **Cost:** The cost of OpioidSafe may be a barrier for some healthcare professionals, particularly those in smaller practices or rural areas.
* **Limited Personalization:** While the platform offers a comprehensive curriculum, it may not be fully tailored to the specific needs of individual healthcare professionals or practice settings.
* **Reliance on Technology:** The online format requires a reliable internet connection and may not be suitable for healthcare professionals with limited access to technology.
* **Lack of Hands-On Experience:** While the platform incorporates simulations and case studies, it cannot fully replicate the hands-on experience of managing patients in real-world clinical settings.
Ideal User Profile
OpioidSafe is best suited for healthcare professionals who are involved in prescribing or dispensing opioid medications, including physicians, nurse practitioners, physician assistants, pharmacists, and dentists. It is particularly beneficial for those who are new to opioid management or who need to update their knowledge on the latest guidelines and best practices.
Key Alternatives
Alternatives to OpioidSafe include live training programs offered by professional organizations, such as the American Medical Association (AMA) and the American Academy of Pain Medicine (AAPM), as well as other online training platforms. These alternatives may offer different features, pricing structures, and levels of personalization.
Expert Overall Verdict & Recommendation
Overall, OpioidSafe is a high-quality DEA opioid training program that offers a comprehensive and engaging learning experience. While it has some limitations, its strengths outweigh its weaknesses, making it a valuable resource for healthcare professionals seeking to enhance their knowledge and skills in opioid management. We recommend OpioidSafe to healthcare professionals who are looking for a convenient and effective way to meet their DEA opioid training requirements.
Insightful Q&A Section
Here are 10 frequently asked questions (FAQs) related to DEA opioid training requirements, along with expert answers:
**Q1: What specific topics must be covered in a DEA-compliant opioid training program?**
**A:** DEA-compliant training must cover comprehensive pain management techniques, opioid pharmacology, risk assessment and mitigation strategies, proper PDMP utilization, diversion control methods, safe storage and disposal practices, and overdose recognition and response protocols. It should also emphasize the importance of MAT for OUD.
**Q2: How often are healthcare professionals required to complete DEA opioid training?**
**A:** The frequency of required DEA opioid training may vary depending on state regulations and individual practice settings. However, it is generally recommended to complete training at least every two to three years to stay current with the latest guidelines and best practices.
**Q3: Are there specific types of healthcare professionals who are exempt from DEA opioid training requirements?**
**A:** While the DEA mandate affects a broad range of prescribers, specific exemptions may apply depending on the state and the nature of the practice. It’s crucial to consult state regulations for precise details on who must comply.
**Q4: Can I complete DEA opioid training online, or must it be done in person?**
**A:** Many DEA-compliant opioid training programs are available online, offering a convenient and flexible way to meet training requirements. However, some states may require a portion of the training to be completed in person.
**Q5: How can I verify that a DEA opioid training program is accredited and meets the necessary requirements?**
**A:** Look for training programs that are accredited by reputable organizations, such as the Accreditation Council for Continuing Medical Education (ACCME) or the American Nurses Credentialing Center (ANCC). These organizations ensure that training programs meet rigorous standards of quality and content.
**Q6: What are the potential consequences of failing to comply with DEA opioid training requirements?**
**A:** Failure to comply with DEA opioid training requirements can result in penalties, such as fines, suspension or revocation of prescribing privileges, and legal repercussions. It can also damage a healthcare professional’s reputation and jeopardize patient safety.
**Q7: How does the DEA opioid training address the issue of implicit bias in pain management?**
**A:** High-quality DEA opioid training programs address the issue of implicit bias by providing education on cultural competency, communication skills, and strategies for addressing disparities in pain management. These programs emphasize the importance of providing equitable and patient-centered care to all individuals, regardless of their race, ethnicity, gender, or socioeconomic status.
**Q8: What resources are available to help healthcare professionals implement best practices in opioid management?**
**A:** Numerous resources are available to support healthcare professionals in implementing best practices in opioid management, including clinical guidelines, practice tools, patient education materials, and continuing education opportunities. These resources can be found on the websites of professional organizations, government agencies, and academic institutions.
**Q9: How can I effectively communicate with patients about the risks and benefits of opioid medications?**
**A:** Effective communication with patients about the risks and benefits of opioid medications involves providing clear, concise, and patient-friendly information. Healthcare professionals should explain the potential side effects of opioids, the risk of addiction, and the importance of safe storage and disposal. They should also encourage patients to ask questions and express any concerns they may have.
**Q10: What is the role of state prescription drug monitoring programs (PDMPs) in preventing opioid misuse and diversion?**
**A:** State PDMPs play a crucial role in preventing opioid misuse and diversion by tracking the prescribing and dispensing of controlled substances. Healthcare professionals can use PDMPs to monitor patient opioid use, identify potential red flags, and prevent doctor shopping. PDMPs also provide valuable data for identifying trends in opioid misuse and diversion, informing public health interventions.
Conclusion & Strategic Call to Action
Navigating the DEA opioid training requirements is essential for all healthcare professionals involved in prescribing or dispensing controlled substances. By understanding the core concepts, adhering to best practices, and seeking out high-quality training programs, you can contribute to combating the opioid crisis and ensuring patient safety. Staying informed, continuously improving your knowledge, and fostering open communication with patients are critical steps in promoting responsible opioid management.
The future of opioid prescribing hinges on informed, responsible practices. Take the next step in enhancing your expertise and demonstrating your commitment to patient safety. Explore accredited DEA opioid training programs in your area and share your experiences or insights in the comments below. Contact our experts for a consultation on developing comprehensive opioid management strategies for your practice.