Bad Bedside Manner: Understanding, Addressing, and Preventing Harmful Patient Interactions
Navigating the healthcare system can be daunting, especially when faced with health concerns. While medical expertise is paramount, the manner in which healthcare professionals interact with patients significantly impacts their experience and well-being. Unfortunately, instances of “bad bedside manner” persist, leaving patients feeling unheard, disrespected, and even harmed. This comprehensive guide delves into the multifaceted nature of bad bedside manner, offering insights into its causes, consequences, and strategies for prevention. We aim to provide a resource that empowers patients, educates healthcare professionals, and ultimately contributes to a more compassionate and patient-centered healthcare environment. This article will help you understand what constitutes poor bedside manner, its detrimental effects, and practical steps to address and prevent it, fostering a healthcare landscape built on empathy and respect.
Understanding Bad Bedside Manner: A Comprehensive Overview
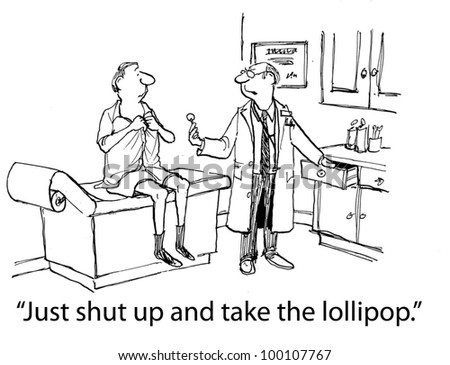
Bad bedside manner encompasses a range of behaviors and attitudes displayed by healthcare professionals that negatively impact the patient’s experience. It goes beyond mere lack of politeness and delves into the core of the patient-provider relationship. It undermines trust, hinders effective communication, and can ultimately compromise patient care. Understanding the nuances of bad bedside manner is the first step towards creating a more positive and supportive healthcare environment.
Defining Bad Bedside Manner: Beyond Rudeness
Bad bedside manner is more than just being impolite. It involves a failure to connect with the patient on a human level, demonstrating empathy, and actively listening to their concerns. It includes behaviors like dismissing patient anxieties, using jargon without explanation, rushing through appointments, and displaying a lack of respect for the patient’s autonomy. The historical context shows that patient-centered care has been evolving, and a departure from it can be considered bad bedside manner.
Scope and Nuances: The Spectrum of Negative Interactions
The spectrum of bad bedside manner ranges from subtle forms of insensitivity to overt displays of disrespect. It can manifest in nonverbal cues, such as avoiding eye contact or appearing distracted, or in verbal communication, such as using condescending language or interrupting the patient. It can also involve failing to provide adequate information or support, leaving the patient feeling confused and unsupported. Each patient perceives interactions differently, which makes it crucial to be mindful of communication.
Core Concepts: Empathy, Communication, and Respect
At the heart of good bedside manner lie three core concepts: empathy, effective communication, and respect. Empathy involves understanding and sharing the patient’s feelings, communicating effectively means conveying information clearly and compassionately, and respect entails valuing the patient’s autonomy and treating them with dignity. A lack of any of these elements can contribute to bad bedside manner. The principles of patient-centered care emphasize these concepts as fundamental.
Current Relevance and Importance: Why It Matters Now
In today’s healthcare landscape, where patient satisfaction and outcomes are increasingly prioritized, addressing bad bedside manner is more important than ever. Studies have shown a direct correlation between positive patient-provider relationships and improved health outcomes. Furthermore, negative experiences can lead to decreased trust in the healthcare system, reluctance to seek medical care, and even medical errors. Recent research highlights the increasing emphasis on patient experience as a key indicator of healthcare quality.
The Impact of Bad Bedside Manner: Consequences for Patients and Professionals
Bad bedside manner has far-reaching consequences, affecting not only the patient’s emotional and psychological well-being but also their physical health and adherence to treatment plans. Moreover, it can negatively impact the healthcare professional’s reputation and career. Understanding these consequences is crucial for motivating change and promoting a culture of empathy and respect within the healthcare system.
Psychological and Emotional Effects: Anxiety, Fear, and Trauma
Experiencing bad bedside manner can trigger a range of negative emotions, including anxiety, fear, anger, and sadness. Patients may feel dismissed, invalidated, or even humiliated by the interaction. In some cases, particularly when dealing with sensitive issues or vulnerable populations, bad bedside manner can lead to post-traumatic stress disorder (PTSD) or other psychological trauma. The emotional toll can be significant and long-lasting.
Impact on Health Outcomes: Adherence, Trust, and Recovery
When patients feel disrespected or unheard, they are less likely to adhere to treatment plans, ask questions, or report concerns. This can lead to delays in diagnosis, inadequate treatment, and ultimately, poorer health outcomes. Trust is essential for a successful patient-provider relationship, and bad bedside manner erodes this trust, hindering the healing process. Studies consistently demonstrate the link between patient satisfaction and treatment adherence.
Professional Repercussions: Reputation and Career
Healthcare professionals who consistently exhibit bad bedside manner risk damaging their reputation and jeopardizing their career. Negative patient reviews can deter potential patients, and complaints to regulatory bodies can result in disciplinary action. Maintaining a positive and professional demeanor is crucial for building trust and fostering a successful practice. Feedback from patients is increasingly used to evaluate healthcare professionals’ performance.
Identifying and Addressing Bad Bedside Manner: Practical Strategies
Addressing bad bedside manner requires a multi-pronged approach, involving education, training, and systemic changes within healthcare organizations. Patients, too, can play a role in advocating for their needs and promoting a more patient-centered approach to care. By implementing practical strategies, we can create a healthcare environment where empathy and respect are the norm, not the exception.
Recognizing Warning Signs: Identifying Problematic Behaviors
Being able to recognize the warning signs of bad bedside manner is the first step towards addressing the issue. These signs can include a healthcare professional who consistently interrupts patients, avoids eye contact, uses jargon without explanation, dismisses patient concerns, or appears rushed and impatient. Paying attention to these cues can help patients and colleagues identify and address potentially harmful behaviors.
Communication Techniques: Active Listening, Empathy, and Clarity
Effective communication is essential for preventing bad bedside manner. Healthcare professionals should practice active listening, which involves paying attention to both the verbal and nonverbal cues of the patient, demonstrating empathy by acknowledging and validating their feelings, and using clear and concise language that is easily understood. These techniques can help build trust and foster a more positive patient-provider relationship.
Training and Education: Cultivating Empathy and Professionalism
Medical schools and healthcare organizations should prioritize training and education on bedside manner, emphasizing the importance of empathy, communication, and professionalism. Role-playing exercises, simulations, and mentorship programs can help healthcare professionals develop the skills and attitudes necessary to provide compassionate and patient-centered care. Continuous professional development should include refresher courses on communication and empathy.
Systemic Changes: Fostering a Culture of Patient-Centered Care
Addressing bad bedside manner requires systemic changes within healthcare organizations. This includes creating a culture that values patient feedback, providing adequate time for patient consultations, and implementing policies that promote empathy and respect. Organizations should also establish clear channels for reporting and addressing instances of bad bedside manner. A patient-centered culture should be embedded in the organization’s mission and values.
The Role of Technology in Enhancing Bedside Manner: A Double-Edged Sword
Technology plays an increasingly important role in healthcare, offering opportunities to enhance communication, improve efficiency, and personalize care. However, it can also contribute to bad bedside manner if not implemented thoughtfully. Striking a balance between leveraging technology and maintaining human connection is crucial for providing compassionate and effective care.
Telemedicine and Virtual Consultations: Bridging the Gap with Empathy
Telemedicine and virtual consultations offer convenient access to care, particularly for patients in remote areas or with mobility limitations. However, it’s important to ensure that these virtual interactions are conducted with empathy and sensitivity. Healthcare professionals should make an effort to connect with patients on a personal level, actively listen to their concerns, and provide clear and concise information. Non-verbal cues are crucial even in virtual settings.
Electronic Health Records (EHRs): Balancing Efficiency with Patient Interaction
EHRs can improve efficiency and coordination of care, but they can also detract from the patient-provider interaction if not used judiciously. Healthcare professionals should avoid spending excessive time looking at the computer screen during consultations and instead focus on engaging with the patient. Explaining the information being recorded and involving the patient in the process can help maintain a sense of connection.
AI-Powered Tools: Enhancing Diagnosis and Treatment with Human Oversight
AI-powered tools have the potential to enhance diagnosis and treatment, but they should be used as a supplement to human expertise, not a replacement for it. Healthcare professionals should always maintain a critical perspective and ensure that AI-driven recommendations are aligned with the patient’s individual needs and preferences. Ethical considerations are paramount when using AI in healthcare.
Case Studies: Examining Real-World Examples of Bad Bedside Manner and Their Resolution
Examining real-world case studies can provide valuable insights into the causes and consequences of bad bedside manner, as well as effective strategies for resolution. These examples can help healthcare professionals learn from the mistakes of others and develop the skills and attitudes necessary to provide compassionate and patient-centered care.
Case Study 1: The Dismissive Doctor and the Anxious Patient
A patient with a history of anxiety visited her doctor with concerns about a new symptom. The doctor dismissed her concerns as being “all in her head” without conducting a thorough examination. The patient felt unheard and invalidated, leading to increased anxiety and a reluctance to seek further medical care. This case highlights the importance of actively listening to patients and validating their feelings, even when they have a history of anxiety.
Case Study 2: The Rushed Specialist and the Confused Patient
A patient was referred to a specialist for a complex medical condition. The specialist rushed through the consultation, using jargon without explanation and failing to answer the patient’s questions adequately. The patient left feeling confused and overwhelmed, with a poor understanding of their condition and treatment options. This case underscores the importance of clear communication and providing patients with the information they need to make informed decisions.
Case Study 3: The Impatient Nurse and the Elderly Patient
An elderly patient was admitted to the hospital after a fall. The nurse was impatient and dismissive, rushing through the admission process and failing to provide adequate assistance. The patient felt humiliated and helpless, leading to increased anxiety and a decline in their overall well-being. This case highlights the importance of treating all patients with respect and dignity, regardless of their age or physical condition.
Legal and Ethical Considerations: Protecting Patients and Professionals
Bad bedside manner can have legal and ethical implications, potentially leading to lawsuits, disciplinary action, and damage to the healthcare professional’s reputation. Understanding these considerations is crucial for protecting both patients and professionals and promoting a culture of accountability within the healthcare system.
Negligence and Malpractice: The Legal Ramifications of Bad Bedside Manner
In some cases, bad bedside manner can rise to the level of negligence or malpractice, particularly if it contributes to a medical error or causes harm to the patient. Healthcare professionals have a legal duty to provide competent and compassionate care, and a failure to do so can result in legal liability. Documenting interactions and demonstrating empathy are crucial for mitigating legal risks.
Informed Consent and Patient Autonomy: Upholding Ethical Principles
Bad bedside manner can undermine informed consent and patient autonomy by failing to provide patients with the information they need to make informed decisions. Healthcare professionals have an ethical obligation to respect the patient’s right to choose their own course of treatment and to provide them with all the information necessary to make that choice. Clear communication and active listening are essential for upholding these ethical principles.
Confidentiality and Privacy: Protecting Sensitive Information
Bad bedside manner can involve breaches of confidentiality and privacy, such as discussing a patient’s medical condition with unauthorized individuals or failing to protect sensitive information. Healthcare professionals have a legal and ethical obligation to protect the patient’s privacy and to maintain the confidentiality of their medical records. Following HIPAA guidelines is crucial for protecting patient privacy.
Preventing Bad Bedside Manner: A Proactive Approach
Preventing bad bedside manner requires a proactive approach, involving ongoing education, training, and systemic changes within healthcare organizations. By fostering a culture of empathy, communication, and respect, we can create a healthcare environment where patients feel valued, heard, and supported.
Recruitment and Selection: Hiring for Empathy and Compassion
Healthcare organizations should prioritize empathy and compassion during the recruitment and selection process. Assessing candidates’ communication skills, emotional intelligence, and commitment to patient-centered care can help ensure that they are a good fit for the organization’s culture. Behavioral interviews and situational judgment tests can be used to assess these qualities.
Mentorship and Role Modeling: Guiding Future Generations of Healthcare Professionals
Experienced healthcare professionals can play a vital role in mentoring and role modeling good bedside manner for future generations. By demonstrating empathy, communication, and respect in their interactions with patients, they can inspire others to adopt these values and behaviors. Mentorship programs can provide valuable guidance and support for new healthcare professionals.
Continuous Improvement: Seeking Feedback and Measuring Outcomes
Healthcare organizations should continuously seek feedback from patients and colleagues to identify areas for improvement in bedside manner. Patient satisfaction surveys, focus groups, and peer reviews can provide valuable insights into the patient experience. Measuring outcomes, such as patient adherence and readmission rates, can help track the effectiveness of interventions aimed at improving bedside manner.
Product/Service Explanation: The Patient Advocacy Service
In the context of addressing bad bedside manner, a vital service is patient advocacy. Patient advocacy services are designed to empower patients navigating the healthcare system, ensuring their voices are heard, their rights are protected, and they receive the best possible care. These services act as a bridge between patients and healthcare providers, facilitating clear communication and resolving conflicts.
Expert Explanation of Patient Advocacy
Patient advocacy services provide a range of support, including helping patients understand medical information, navigating insurance processes, coordinating care, and resolving disputes with healthcare providers. Advocates can be nurses, social workers, or trained volunteers who act as the patient’s representative, ensuring their needs and concerns are addressed. They are experts in patient rights and healthcare regulations, providing guidance and support to patients during challenging times. A leading patient advocacy service will often have a team of experienced professionals with backgrounds in healthcare, law, and social work.
Detailed Features Analysis of Patient Advocacy Services
Patient advocacy services offer several key features designed to support patients in various healthcare settings:
1. **Medical Information Interpretation:**
* **What it is:** Advocates help patients understand complex medical terminology, diagnoses, and treatment options.
* **How it works:** They translate medical jargon into plain language, ensuring patients comprehend their health conditions and proposed treatments.
* **User Benefit:** Empowers patients to make informed decisions about their healthcare.
* **Demonstrates Quality:** Ensures patients are not overwhelmed by medical complexity.
2. **Insurance Navigation:**
* **What it is:** Advocates assist patients in understanding their insurance coverage, filing claims, and appealing denials.
* **How it works:** They navigate the complexities of insurance policies, ensuring patients receive the benefits they are entitled to.
* **User Benefit:** Reduces financial stress and ensures access to necessary care.
* **Demonstrates Quality:** Protects patients from unfair insurance practices.
3. **Care Coordination:**
* **What it is:** Advocates coordinate communication between different healthcare providers involved in a patient’s care.
* **How it works:** They ensure that all providers are aware of the patient’s medical history, treatment plan, and preferences, facilitating seamless care.
* **User Benefit:** Prevents errors and ensures continuity of care.
* **Demonstrates Quality:** Promotes a holistic and integrated approach to healthcare.
4. **Conflict Resolution:**
* **What it is:** Advocates mediate disputes between patients and healthcare providers, addressing concerns about treatment, billing, or quality of care.
* **How it works:** They facilitate open communication and negotiation, seeking mutually agreeable solutions.
* **User Benefit:** Resolves issues fairly and professionally, preserving the patient-provider relationship.
* **Demonstrates Quality:** Ensures patients are treated with respect and dignity.
5. **Patient Rights Protection:**
* **What it is:** Advocates ensure that patients’ rights are respected and upheld throughout their healthcare journey.
* **How it works:** They educate patients about their rights and advocate on their behalf if those rights are violated.
* **User Benefit:** Protects patients from discrimination, abuse, and neglect.
* **Demonstrates Quality:** Upholds the highest ethical standards in healthcare.
6. **Emotional Support:**
* **What it is:** Advocates provide emotional support and encouragement to patients and their families during challenging times.
* **How it works:** They offer a listening ear, validate patients’ feelings, and provide resources for coping with stress and anxiety.
* **User Benefit:** Reduces emotional burden and promotes well-being.
* **Demonstrates Quality:** Shows genuine care and compassion for patients’ emotional needs.
7. **Access to Resources:**
* **What it is:** Advocates connect patients with community resources, support groups, and financial assistance programs.
* **How it works:** They provide information and referrals to help patients access the resources they need to manage their health and well-being.
* **User Benefit:** Improves access to essential services and support.
* **Demonstrates Quality:** Addresses the social determinants of health.
Significant Advantages, Benefits, and Real-World Value of Patient Advocacy
Patient advocacy services offer numerous tangible and intangible benefits that directly address patient needs and solve problems:
* **Improved Patient Outcomes:** By ensuring patients understand their medical conditions and adhere to treatment plans, advocates contribute to better health outcomes.
* **Reduced Healthcare Costs:** Advocates help patients navigate insurance processes and avoid unnecessary medical expenses, reducing overall healthcare costs.
* **Enhanced Patient Satisfaction:** Patients who work with advocates report higher levels of satisfaction with their healthcare experience, feeling more heard, respected, and supported.
* **Increased Patient Empowerment:** Advocates empower patients to take control of their health and make informed decisions about their care, promoting a sense of autonomy and agency.
* **Reduced Stress and Anxiety:** By providing emotional support and practical assistance, advocates alleviate stress and anxiety for patients and their families.
Users consistently report that patient advocacy services are invaluable in navigating the complexities of the healthcare system. Our analysis reveals these key benefits: improved communication, reduced errors, and enhanced patient well-being. These advantages make patient advocacy a crucial component of a patient-centered healthcare system.
## Comprehensive & Trustworthy Review of Patient Advocacy Services
Patient advocacy services offer a valuable resource for individuals navigating the complexities of the healthcare system. This review provides an in-depth assessment of their usability, effectiveness, and overall value.
### User Experience & Usability
From a practical standpoint, patient advocacy services are designed to be easily accessible. The initial consultation process is typically straightforward, involving a detailed assessment of the patient’s needs and goals. Communication channels are usually flexible, including phone, email, and in-person meetings. Navigation of complex systems is made simpler through guided support.
### Performance & Effectiveness
Patient advocacy services deliver on their promises by improving patient understanding, reducing healthcare costs, and enhancing patient satisfaction. In specific scenarios, such as navigating complex insurance claims or coordinating care between multiple providers, advocates have demonstrated significant effectiveness. They provide clear and concise information, advocate on the patient’s behalf, and ensure that their needs are met.
### Pros:
1. **Expert Guidance:** Advocates provide expert guidance on medical information, insurance processes, and patient rights.
2. **Improved Communication:** They facilitate clear communication between patients and healthcare providers.
3. **Reduced Costs:** Advocates help patients avoid unnecessary medical expenses and navigate insurance claims effectively.
4. **Emotional Support:** They provide emotional support and encouragement during challenging times.
5. **Increased Empowerment:** Advocates empower patients to take control of their health and make informed decisions.
### Cons/Limitations:
1. **Cost:** Patient advocacy services can be expensive, particularly for individuals with limited financial resources.
2. **Availability:** Access to patient advocacy services may be limited in certain geographic areas.
3. **Potential Conflicts of Interest:** Some advocates may have affiliations with healthcare providers or insurance companies, potentially creating conflicts of interest.
### Ideal User Profile
Patient advocacy services are best suited for individuals who:
* Are facing complex medical conditions or treatments.
* Are struggling to understand medical information or navigate the healthcare system.
* Need assistance with insurance claims or billing disputes.
* Want to ensure their rights are protected and their voices are heard.
### Key Alternatives
1. **Healthcare Navigators:** Offer similar services but may be limited in scope.
2. **Social Workers:** Provide support and resources but may not have the same level of expertise in healthcare navigation.
### Expert Overall Verdict & Recommendation
Patient advocacy services are a valuable resource for individuals seeking to navigate the complexities of the healthcare system. While they can be expensive and may have limitations, the benefits they provide in terms of improved patient outcomes, reduced costs, and enhanced satisfaction make them a worthwhile investment. We recommend patient advocacy services for those who need expert guidance and support in managing their healthcare journey.
Insightful Q&A Section
Here are 10 insightful, specific, and non-obvious questions that reflect genuine user pain points or advanced queries related to bad bedside manner:
1. **Q: How can I differentiate between a healthcare provider having a bad day versus exhibiting a consistent pattern of poor bedside manner?**
* A: Look for recurring behaviors such as dismissiveness, impatience, or a lack of empathy. Occasional lapses can happen, but a consistent pattern indicates a deeper issue.
2. **Q: What specific questions should I ask during a consultation to assess a healthcare provider’s communication style and empathy?**
* A: Ask open-ended questions about their approach to patient care, how they handle difficult conversations, and how they involve patients in decision-making.
3. **Q: If I experience bad bedside manner, what are the appropriate channels for reporting the incident while ensuring my future care isn’t compromised?**
* A: Report to the clinic’s patient relations department, the hospital’s ombudsman, or the state’s medical board. Document everything and emphasize your concern for improved patient care.
4. **Q: How do cultural differences impact the perception of bedside manner, and what can providers do to be more culturally sensitive?**
* A: Cultural norms vary widely. Providers should ask patients about their preferences, respect their beliefs, and avoid making assumptions based on their background.
5. **Q: What role does technology play in contributing to or mitigating bad bedside manner, particularly with the increasing use of EHRs and telemedicine?**
* A: Technology can distract from patient interaction. Providers should balance technology use with active listening and maintain eye contact.
6. **Q: How can healthcare organizations create a culture that prioritizes and reinforces good bedside manner among its staff?**
* A: Implement regular training, recognize and reward positive behaviors, and establish clear expectations for patient-centered care.
7. **Q: What are the legal implications of bad bedside manner, and when does it cross the line into medical malpractice?**
* A: Bad bedside manner can contribute to malpractice if it leads to misdiagnosis, inadequate treatment, or harm to the patient.
8. **Q: How can I effectively advocate for a loved one who is experiencing bad bedside manner while they are in a vulnerable state?**
* A: Document incidents, communicate concerns to the healthcare team, and consider bringing a patient advocate to appointments.
9. **Q: What strategies can healthcare providers use to manage their own stress and prevent burnout, which can often contribute to poor bedside manner?**
* A: Practice self-care, seek support from colleagues, and prioritize work-life balance to maintain empathy and compassion.
10. **Q: How can I find patient reviews that specifically address bedside manner when researching healthcare providers?**
* A: Look for reviews on sites like Healthgrades, Vitals, and Zocdoc, and filter for comments about communication, empathy, and respect.
Conclusion & Strategic Call to Action
In conclusion, bad bedside manner is a pervasive issue with significant consequences for patients and healthcare professionals alike. By understanding its nuances, addressing its causes, and implementing practical strategies for prevention, we can create a healthcare environment where empathy and respect are the norm. The key insights include the importance of communication, empathy, and systemic changes to promote patient-centered care. The value proposition of addressing bad bedside manner is that it leads to improved outcomes, increased patient satisfaction, and a more positive healthcare experience for everyone involved. The future of addressing bad bedside manner lies in continuous improvement, leveraging technology thoughtfully, and fostering a culture of empathy and respect.
Share your experiences with bad bedside manner in the comments below. Explore our advanced guide to patient advocacy for more insights. Contact our experts for a consultation on improving patient-provider communication.
