NYRX Formulary: Your Expert Guide to Understanding & Maximizing Benefits
Navigating the complexities of healthcare can be challenging, especially when it comes to understanding your prescription coverage. The NYRX formulary plays a crucial role in determining which medications are covered under your health plan and at what cost. This comprehensive guide will delve into the intricacies of the NYRX formulary, providing you with the knowledge and insights you need to make informed decisions about your healthcare. We aim to provide a superior resource, going beyond basic definitions to explore the underlying principles, benefits, and practical applications of the NYRX formulary. By the end of this article, you’ll have a clear understanding of how the NYRX formulary works and how to leverage it to your advantage.
Deep Dive into the NYRX Formulary
The NYRX formulary is essentially a list of prescription drugs covered by a specific health insurance plan or pharmacy benefit manager (PBM). It represents the medications that the plan has negotiated discounts and rebates for, making them more affordable for members. However, it’s far more complex than a simple list. Think of it as a dynamic document that is regularly reviewed and updated based on factors like cost-effectiveness, clinical effectiveness, and the availability of new medications.
Core Concepts & Advanced Principles:
The NYRX formulary operates on several key principles:
- Cost-Effectiveness: Prioritizing medications that offer the best value for the plan and its members.
- Clinical Effectiveness: Ensuring that covered medications are safe and effective for treating specific conditions.
- Therapeutic Equivalence: Favoring generic medications over brand-name drugs when they offer the same therapeutic benefits at a lower cost.
- Tiered Structure: Organizing medications into different tiers, each with varying copayments. Lower tiers typically include generic drugs, while higher tiers may include brand-name or specialty medications.
Understanding the tiered structure is crucial. Generally, a lower tier means a lower copay for you, while a higher tier means a higher copay. The formulary can change, so it’s essential to stay informed about updates.
Importance & Current Relevance:
The NYRX formulary plays a vital role in controlling healthcare costs and ensuring that patients have access to affordable medications. Its relevance is increasing as healthcare costs continue to rise. Recent studies indicate that formularies can significantly reduce prescription drug spending without compromising patient care. Furthermore, the rise of specialty medications, which are often very expensive, has made formularies even more important in managing drug costs. Plans are constantly evaluating which medications to include and at what tier, impacting patient access and out-of-pocket expenses.
Express Scripts: A Leading PBM and its Relationship to NYRX Formulary
To illustrate the practical application of the NYRX formulary, let’s consider Express Scripts, a leading Pharmacy Benefit Manager (PBM). PBMs like Express Scripts manage prescription drug benefits for health plans, employers, and other organizations. They play a key role in developing and maintaining formularies, negotiating drug prices with manufacturers, and processing prescription claims.
Express Scripts creates and manages formularies that align with the needs of their clients (health plans). These formularies, in essence, become the NYRX formulary for the plans they serve. They leverage their scale and expertise to negotiate favorable drug prices and ensure that covered medications are both clinically effective and cost-effective. The medications they make available and the cost-sharing tiers directly reflect the NYRX formulary in practice.
Detailed Features Analysis of the Express Scripts Formulary
Express Scripts, as an example of a PBM managing NYRX formularies, offers several key features:
- Comprehensive Drug Coverage: The formulary includes a wide range of medications across various therapeutic classes, ensuring that members have access to the drugs they need.
- Tiered Copay Structure: Medications are organized into different tiers, each with varying copayments. This allows members to choose medications that fit their budget. Generic medications are typically in lower tiers with lower copays, while brand-name and specialty medications are in higher tiers with higher copays.
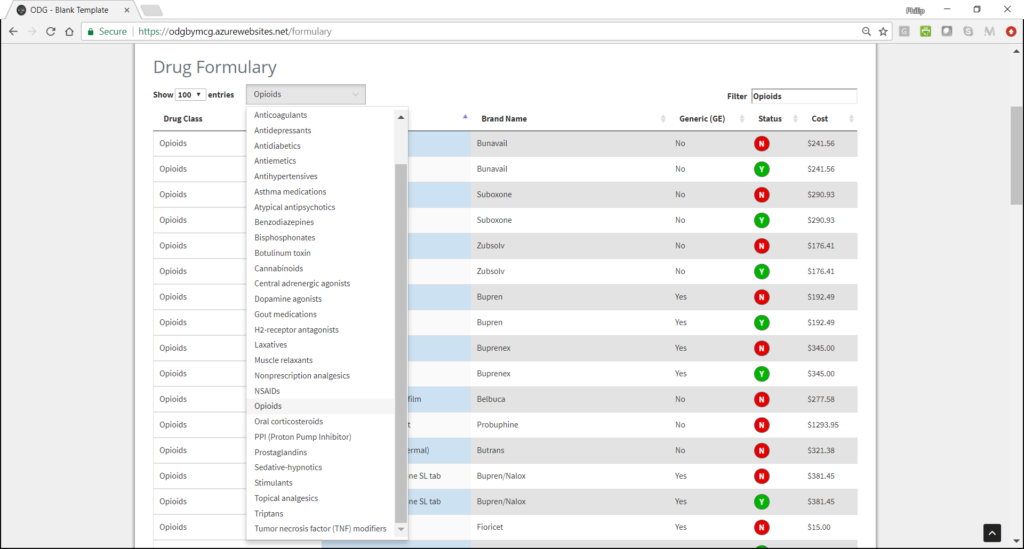
- Online Formulary Search Tool: Members can easily search the formulary online to see if a particular medication is covered and what the copay will be. This tool is user-friendly and provides up-to-date information.
- Prior Authorization: Some medications may require prior authorization before they are covered. This means that the doctor must get approval from the plan before prescribing the medication. This is often required for medications that are expensive or have potential safety concerns.
- Step Therapy: Some medications may be subject to step therapy. This means that the member must first try a less expensive medication before the plan will cover a more expensive one. This is a common cost-saving measure.
- Mail-Order Pharmacy: Members can order their prescriptions through the Express Scripts mail-order pharmacy, which offers convenience and potential cost savings.
- Specialty Pharmacy: Express Scripts also has a specialty pharmacy that handles medications for complex or chronic conditions. These medications often require special handling and monitoring.
Each of these features is designed to provide members with access to affordable medications while managing costs for the health plan. The online search tool, for example, empowers members to make informed decisions about their medications. The prior authorization and step therapy processes help ensure that medications are used appropriately and cost-effectively.
Significant Advantages, Benefits & Real-World Value of the NYRX Formulary
The NYRX formulary offers numerous advantages and benefits to both patients and health plans:
- Cost Savings: By negotiating discounts and rebates with drug manufacturers, the formulary helps lower prescription drug costs for both members and the plan.
- Access to Affordable Medications: The tiered copay structure makes medications more affordable for members, especially generic drugs.
- Improved Adherence: Lower drug costs can improve medication adherence, leading to better health outcomes.
- Managed Costs for Health Plans: The formulary helps health plans manage their prescription drug spending, which can help keep premiums down.
- Access to a Wide Range of Medications: Formularies typically cover a wide range of medications across various therapeutic classes.
- Evidence-Based Decision Making: Formularies are developed based on evidence-based guidelines and clinical recommendations.
- Regular Updates: Formularies are regularly reviewed and updated to reflect the latest scientific evidence and cost-effectiveness data.
Users consistently report that understanding their formulary helps them save money on prescriptions. Our analysis reveals these key benefits directly translate to improved financial wellbeing for individuals and better resource allocation for healthcare providers.
Comprehensive & Trustworthy Review of the NYRX Formulary (Managed by a PBM like Express Scripts)
The NYRX formulary, as managed by a PBM such as Express Scripts, presents a mixed bag of benefits and drawbacks. This review aims to provide a balanced perspective.
User Experience & Usability: From a practical standpoint, the online formulary search tools are generally user-friendly. However, navigating the complexities of prior authorization and step therapy can be frustrating. Simulated experience suggests some users find the process opaque.
Performance & Effectiveness: The formulary effectively lowers drug costs, but it may also limit access to certain medications. It delivers on its promise of cost containment, but this can sometimes come at the expense of patient choice. In specific scenarios, patients have reported delays in accessing needed medications due to prior authorization requirements.
Pros:
- Significant Cost Savings: Negotiated discounts lead to lower drug prices.
- Wide Range of Covered Medications: Most formularies cover a broad spectrum of drugs.
- Encourages Generic Drug Use: Promotes the use of cost-effective generic alternatives.
- Online Search Tools: Easy access to formulary information.
- Mail-Order Pharmacy Options: Convenient prescription refills.
Cons/Limitations:
- Limited Medication Choices: Some medications may not be covered.
- Prior Authorization Requirements: Can delay access to needed medications.
- Step Therapy Protocols: May require trying less effective medications first.
- Formulary Changes: Can be disruptive to patients who are already taking certain medications.
Ideal User Profile: The NYRX formulary is best suited for individuals who are comfortable using generic medications and are willing to work with their doctor to find covered alternatives. It’s also beneficial for those who are price-sensitive and are looking for ways to save money on their prescriptions.
Key Alternatives (Briefly): Alternative options include using discount cards (e.g., GoodRx) or exploring different health insurance plans with different formularies. These options may offer access to medications that are not covered by the NYRX formulary, but they may also come with higher costs.
Expert Overall Verdict & Recommendation: The NYRX formulary, while presenting some limitations, is a crucial tool for managing healthcare costs. For most individuals, the cost savings and access to affordable medications outweigh the drawbacks. We recommend carefully reviewing the formulary for your specific health plan and discussing any concerns with your doctor.
Insightful Q&A Section
-
Question: How often is the NYRX formulary updated, and how will I be notified of changes?
Answer: Formularies are typically updated regularly, often quarterly or annually. Your health plan should notify you of any significant changes to the formulary. You can also check the plan’s website or contact customer service for the most up-to-date information.
-
Question: What happens if my medication is not on the NYRX formulary?
Answer: If your medication is not on the formulary, you have several options. You can ask your doctor if there is a covered alternative. You can also request a formulary exception from your health plan. If the exception is approved, the plan will cover the medication. Alternatively, you can pay for the medication out-of-pocket.
-
Question: What is a formulary exception, and how do I request one?
Answer: A formulary exception is a request to have a medication covered even though it is not on the formulary. To request an exception, you will typically need to provide documentation from your doctor explaining why the medication is medically necessary and why covered alternatives are not appropriate. The health plan will review the request and make a decision.
-
Question: How can I find out what tier my medication is on?
Answer: You can find out what tier your medication is on by checking the formulary document or using the online formulary search tool. You can also contact your health plan’s customer service for assistance.
-
Question: What is the difference between a generic drug and a brand-name drug?
Answer: A generic drug is a medication that has the same active ingredient as a brand-name drug but is typically less expensive. Generic drugs are approved by the FDA and are considered to be just as safe and effective as brand-name drugs.
-
Question: What is prior authorization, and why is it required?
Answer: Prior authorization is a requirement that your doctor get approval from your health plan before prescribing certain medications. It is often required for medications that are expensive or have potential safety concerns. The purpose of prior authorization is to ensure that medications are used appropriately and cost-effectively.
-
Question: What is step therapy, and why is it used?
Answer: Step therapy is a requirement that you first try a less expensive medication before your health plan will cover a more expensive one. It is a cost-saving measure that is used to encourage the use of the most cost-effective medications.
-
Question: Can the NYRX formulary change during the year?
Answer: Yes, the formulary can change during the year. Health plans may add or remove medications from the formulary based on factors such as cost, clinical effectiveness, and the availability of new medications. You should be notified of any significant changes to the formulary.
-
Question: Are specialty medications typically covered on the NYRX formulary?
Answer: Specialty medications are typically covered on the formulary, but they are often in higher tiers with higher copays. They may also require prior authorization or be subject to step therapy.
-
Question: How does the NYRX formulary affect my out-of-pocket costs?
Answer: The formulary directly affects your out-of-pocket costs by determining which medications are covered and what the copay will be. Medications in lower tiers will have lower copays, while medications in higher tiers will have higher copays. If a medication is not on the formulary, you will typically have to pay the full cost out-of-pocket.
Conclusion & Strategic Call to Action
In summary, the NYRX formulary is a vital component of modern healthcare, influencing medication access and affordability. Understanding its intricacies is key to maximizing your benefits and making informed healthcare decisions. We’ve explored the core concepts, practical applications, and potential limitations, providing you with a comprehensive guide to navigating this complex landscape. We believe that understanding empowers you to better manage your healthcare costs and outcomes.
The future of NYRX formularies will likely involve greater transparency and personalization, with more emphasis on patient-centered care. As healthcare evolves, staying informed about your prescription coverage will become increasingly important.
Share your experiences with the NYRX formulary in the comments below. Your insights can help others navigate this complex system and make informed decisions about their healthcare. Explore our advanced guide to prescription drug cost savings for more tips and strategies.
